Highlight
– OTOF-targeted inner-ear gene therapy produced measurable hearing restoration and faster improvements in auditory-speech measures than cochlear implantation (CI) over 12 months in a matched cohort study.
– Gene therapy recipients showed better speech-in-noise performance and superior music pitch perception when combined with a contralateral CI versus bilateral CI.
– Early results are promising but limited by small sample size, nonrandomized design, single-center setting, and short follow-up; longer-term safety and durability data are required before replacing CI as the standard of care.
Background
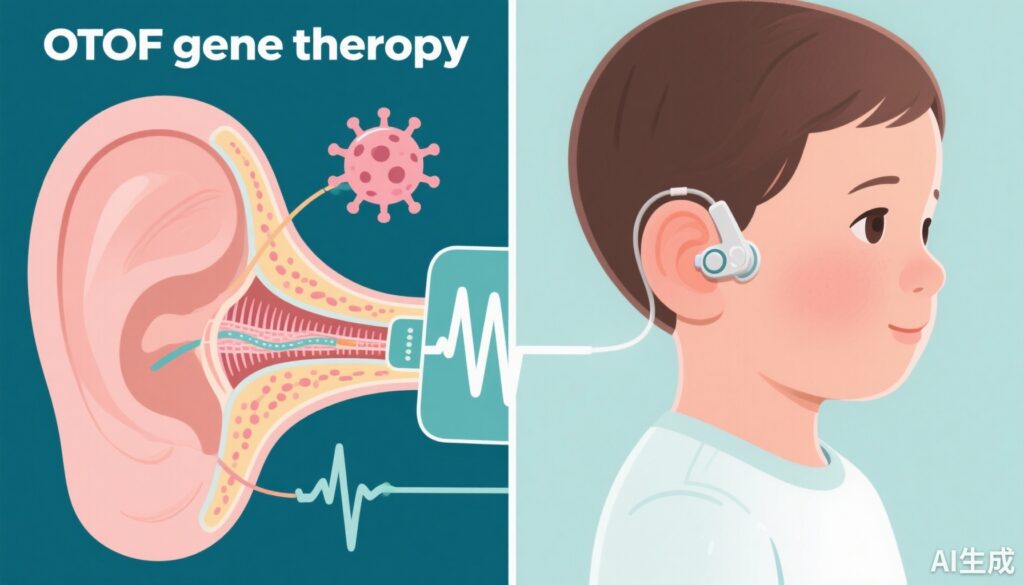
Congenital sensorineural deafness is heterogeneous in etiology; a substantial fraction has a monogenic basis. Mutations in OTOF (encoding otoferlin) cause auditory synaptopathy—severe-to-profound congenital deafness characterized by preserved outer-hair-cell function but impaired synaptic neurotransmission at inner hair cell–auditory nerve synapses. Cochlear implantation (CI) has been the standard treatment for severe-to-profound congenital deafness, restoring access to sound by directly stimulating the auditory nerve and enabling speech and language development. However, CI provides an electroacoustic approximation of hearing with limits in spectral resolution and fine temporal coding, which can affect speech in noise and music perception.
Advances in inner-ear gene transfer technology—viral vectors, delivery techniques, and transgene engineering—have enabled targeted therapies for genetically defined deafness. OTOF is a compelling target because otoferlin is essential for vesicle exocytosis at the inner hair cell synapse; replacing a defective gene could, in principle, restore natural cochlear processing and better fidelity for temporal cues critical for speech-in-noise and music.
Study design
Cheng and colleagues (JAMA Neurol 2025) report a nonblinded cohort study conducted at a single tertiary hospital in China between December 2022 and November 2024 that compared clinical outcomes after OTOF-directed gene therapy (GT) versus cochlear implantation (CI) in children with congenital severe-to-complete hearing loss. Participants were aged 1–18 years and selected to exclude inner-ear malformations and VIII-nerve abnormalities. Investigators screened 1,568 candidates and enrolled 72 patients matched on presurgical hearing thresholds, duration of deafness, and baseline speech ability.
The analytic groups included GT-only, CI-only, and combination (bimodal: unilateral GT + contralateral CI versus bilateral CI). GT recipients underwent inner-ear vector delivery and were followed at 3, 6, and 12 months; CI recipients had evaluations corresponding to those time frames (single-point evaluations at 3, 6, or 12 months). Primary auditory and speech outcomes comprised objective measures (audiometry, auditory brainstem response [ABR]) and functional assessments (IT-MAIS/MAIS, speech and music perception tests). A key neurophysiological secondary measure was mismatch negativity (MMN), an event-related potential indexing cortical auditory discrimination and early auditory processing.
Key findings
Population: 11 GT patients (mean age 3.7 years) and 61 CI patients (mean age 1.9 years) were included. Notably, the GT group was older on average, which bears on developmental plasticity and interpretation of language outcomes.
Hearing thresholds and ABR: In 9 GT patients with available data at 12 months, ABR thresholds improved substantially from >95 dB nHL (baseline) to a mean of 54.8 (SD 15.9) dB nHL at 12 months, indicating partial restoration of auditory sensitivity but not normalization to typical hearing ranges.
Functional auditory and speech outcomes: GT patients demonstrated faster and larger improvements in the IT-MAIS/MAIS scale. At 6 months, median IT-MAIS/MAIS was 31.0 (IQR 30.0–32.0) in the GT cohort versus 23.5 (19.0–26.3) in CI recipients (P = .01). At 12 months the advantage persisted: median 32.0 (31.0–32.0) for GT vs 28.0 (24.5–30.5) for CI (P = .007). These differences indicate earlier gains in meaningful auditory integration and responsiveness to sound among GT recipients.
Auditory cortical processing (MMN): At 6 months, GT-treated patients showed shorter MMN latencies (median 0.20 s [IQR 0.05–0.21]) versus CI patients (median 0.23 s [0.22–0.25]; P = .006), suggesting faster or more natural central auditory discrimination after GT. In bimodal comparisons at 12 months, GT + CI had shorter MMN latencies (median 0.08 s [0.07–0.10]) than bilateral CI (median 0.21 s [0.15–0.23]; P = .01).
Speech in noise and music perception: Bimodal patients with GT (CI off) outperformed unilateral CI patients in disyllable speech-in-noise testing at 12 months (median –1.0 dB SPL [IQR –3.0 to 2.4] vs 5.3 dB SPL [3.1–12.1]; P = .03), implying superior signal extraction in noisy environments. GT + CI patients also achieved higher in-tune singing rates than bilateral CI (median 66.6% [53.7–83.9%] vs 37.1% [30.3–56.3%]; P = .04), suggesting better pitch perception and musical processing when a physiologic hearing pathway is at least partly restored on one side.
Safety and durability: The report focuses on efficacy endpoints through 12 months; the paper does not present detailed long-term safety or immunologic data in this summary. The authors report that GT produced stable hearing recovery during follow-up, but systematic adverse-event tables and long-term durability beyond 12 months remain to be reported or confirmed in larger cohorts.
Effect sizes and statistical considerations
Statistically significant differences (P values 0.01 to 0.04) favor GT for several outcomes; however, effect-size reporting beyond medians and IQRs is limited in the summary. The GT sample (n=11) is small, raising concerns about precision, type I/II error risk, and robustness of subgroup comparisons (e.g., bimodal vs bilateral CI). Matching on baseline hearing and speech ability partially mitigates confounding, but the nonrandomized, single-center design leaves residual potential for selection bias and unmeasured confounders.
Expert commentary and interpretation
This study provides important early clinical evidence that restoring OTOF function via gene therapy can yield not just audibility gains but also faster and, in some domains, superior central auditory processing and perceptual outcomes compared with CI. The biological plausibility is strong: otoferlin replacement should restore neurotransmitter release at inner hair cell synapses, preserving natural cochlear micromechanics and temporal coding—features that underlie speech-in-noise discrimination and pitch perception more effectively than electrical stimulation alone.
However, the study’s limitations temper enthusiasm and mandate cautious interpretation. Key limitations include small GT sample size, nonrandomized allocation, single-center recruitment, and relatively short follow-up. The GT group’s older mean age could influence neural plasticity; early implantation or auditory stimulation is typically associated with better language outcomes, so the observed GT advantage despite older age is notable but requires careful scrutiny for selection bias (for example, children with certain clinical features or family preferences may have been steered to GT). Important safety endpoints—immunologic responses to vectors, otologic complications, off-target effects, and long-term transgene expression—require larger prospective trials and longer observation.
From a practical perspective, translating these results into practice will require standardized genetic screening pathways to identify OTOF mutations, regulatory approval, infrastructure for inner-ear gene delivery, and clear criteria to choose GT alone, CI alone, or combination approaches. The data suggest a potential role for bimodal hearing (physiologic GT on one side with a CI on the other) to leverage both natural temporal fidelity and CI-driven audibility across frequencies.
Where do CIs still fit?
CI remains the established and life-changing treatment for most children with congenital severe-to-profound deafness today, with decades of robust outcome data for speech and language acquisition when implanted early. The present findings do not yet supersede CI as the standard of care but point to GT as an emerging alternative or adjunct for genetically defined subgroups—particularly OTOF-mediated auditory synaptopathy—where restoration of inner hair cell synaptic function would be expected to offer physiologic advantages.
Conclusions and next steps
Cheng et al. report promising early clinical outcomes for OTOF gene therapy in congenital deafness, with earlier gains in functional hearing, faster cortical processing, and advantages in speech-in-noise and music perception—especially in bimodal configurations—compared with cochlear implantation. These data support further development of genotype-guided therapeutics for deafness and reinforce the importance of routine genetic diagnosis in pediatric hearing loss.
Critical next steps include randomized (or rigorously matched prospective) trials with larger samples, multicenter enrollment for external validity, comprehensive safety monitoring, and longer-term follow-up to establish durability of effect. Health economic analyses and pathway design for testing, counseling, and choosing between GT, CI, or combined strategies will be necessary before wide adoption. Finally, integration with early-detection and language-intervention programs is essential because auditory experience during critical windows profoundly shapes language outcomes.
Funding and clinicaltrials.gov
Funding and trial registration details are reported in Cheng et al., JAMA Neurol. 2025. Readers should consult the original article for specific sponsor, grant, and registration identifiers.
References
1. Cheng X, Zhong J, Zhang J, et al. Gene Therapy vs Cochlear Implantation in Restoring Hearing Function and Speech Perception for Individuals With Congenital Deafness. JAMA Neurol. 2025;82(9):941-951. doi:10.1001/jamaneurol.2025.2053 IF: 21.3 Q1
2. World Health Organization. Deafness and hearing loss. WHO; 2021. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
3. Wilson BS, Dorman MF. Cochlear implants: a remarkable past and a brilliant future. Hear Res. 2008;242(1-2):3-21. doi:10.1016/j.heares.2008.06.005 IF: 2.5 Q1