Background and Aims
Celiac disease (CD) is an autoimmune disorder triggered by gluten ingestion, leading to intestinal inflammation and damage. The current standard treatment is a lifelong gluten-free diet (GFD), which aims to reduce symptoms and intestinal damage. However, the effects of CD and sustained gluten avoidance on gut function and the gut microbiome remain incompletely understood. This observational cohort study was designed to investigate how newly diagnosed CD patients’ gut physiology and microbial communities change after one year on a GFD.
Methods
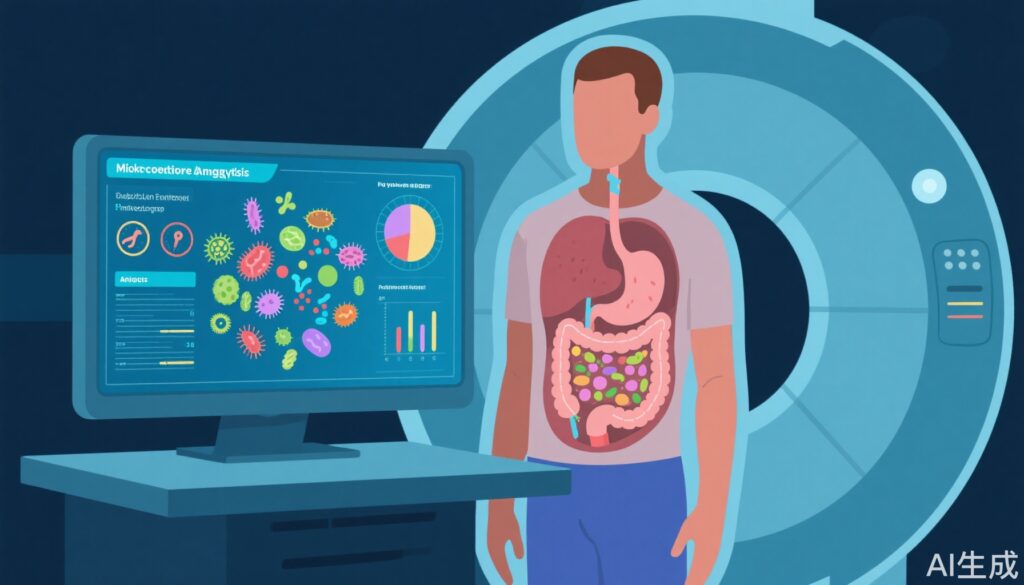
The study enrolled 36 newly diagnosed celiac disease patients alongside 36 healthy volunteers (HVs) as controls. Each participant was evaluated at baseline (diagnosis) and after 12 months of following a gluten-free diet. Key gut function measurements included small bowel water content (SBWC), whole gut transit time (WGTT), and colon volumes, all assessed through magnetic resonance imaging (MRI).
For microbiome analysis, DNA was extracted from stool samples and subjected to shotgun metagenomic sequencing. This approach allowed for detailed profiling of bacterial species and their gene functions, notably carbohydrate active enzymes (CAZymes), which are important for digesting complex carbohydrates.
Results
At baseline, people with celiac disease showed significantly higher small bowel water content (157 ± 15 mL) compared to healthy volunteers (100 ± 12 mL) (P = .003). Their whole gut transit time was also notably delayed (68 ± 8 hours vs. 41 ± 5 hours; P = .002), indicating slower gut motility. After 12 months on a gluten-free diet, these differences decreased but not to a statistically significant extent.
Participants with CD reported a significant improvement in overall well-being after the diet intervention. However, their well-being scores did not fully reach those of the control group.
The gut microbiota in CD patients was characterized by a high abundance of proteolytic gene functions, linked to bacteria such as Escherichia coli, Enterobacter, and Peptostreptococcus. In response to the gluten-free diet, levels of beneficial bifidobacteria significantly decreased, while Blautia wexlerae increased.
Microbiome composition showed positive correlations with delayed gut transit time, increased colon volume, and presence of Akkermansia muciniphila, but negative correlation with Blautia wexlerae. Notably, the reduction in gut transit time and colon volume following the gluten-free diet was significantly associated with an increased abundance of B. wexlerae.
Additionally, the profile of carbohydrate-active enzymes changed significantly, particularly in families responsible for degrading starch and arabinoxylan—components of wheat fiber that are reduced in a gluten-free diet.
Conclusions
Celiac disease alters gut function and the composition of the intestinal microbiome, including microbial genes involved in protein degradation. Adhering to a gluten-free diet for one year improves but does not fully normalize these alterations. A notable consequence of the diet is a significant reduction in bifidobacteria, which is linked to decreased consumption of resistant starch and arabinoxylan—fibers commonly found in wheat.
These findings highlight the complex interplay between diet, gut physiology, and microbiome in celiac disease, suggesting that while a gluten-free diet alleviates symptoms and some gut dysfunction, additional dietary strategies may be needed to fully restore gut microbial balance.
Clinical Implications and Further Research
Clinicians managing celiac disease should be aware that while the gluten-free diet is essential for symptom control and intestinal healing, its impact on gut microbiota could have long-term consequences. Supplementing a gluten-free diet with prebiotics or probiotics targeting beneficial bacteria such as bifidobacteria might support gut health.
Future research should explore tailored dietary interventions that compensate for the reduction in fibers like resistant starch and arabinoxylan to optimize microbiome recovery. Understanding how microbiome changes influence clinical outcomes can guide more comprehensive management of celiac disease.
Reference
Costigan CM, Warren FJ, Duncan AP, Hoad CL, Lewis N, Hill T, Crooks CJ, Morgan PS, Ciacci C, Iovino P, Sanders DS, Hildebrand F, Gowland PA, Spiller RC, Marciani L. One Year of Gluten-Free Diet Impacts Gut Function and Microbiome in Celiac Disease. Clinical Gastroenterology and Hepatology. 2025 Aug;23(9):1525-1534.e14. doi: 10.1016/j.cgh.2024.11.006. Epub 2024 Dec 9. PMID: 39662692.