Background
Ischemic stroke remains a leading cause of mortality and morbidity worldwide, presenting significant challenges in acute management and prognostication. Early identification of patients at elevated risk of mortality is essential to optimize clinical care and resource allocation. Among emerging biomarkers, N-terminal pro-B-type natriuretic peptide (NT-proBNP), traditionally used in cardiology to assess myocardial stress, has shown promise in predicting adverse outcomes after ischemic stroke. Its elevation potentially reflects underlying cardiac dysfunction or systemic stress responding to cerebral ischemia, providing an integrated measure of cardiovascular and cerebrovascular pathology.
Although prior individual studies have suggested NT-proBNP’s association with mortality risk, a comprehensive synthesis of its prognostic accuracy in ischemic stroke is needed to inform clinical application.
Study Design
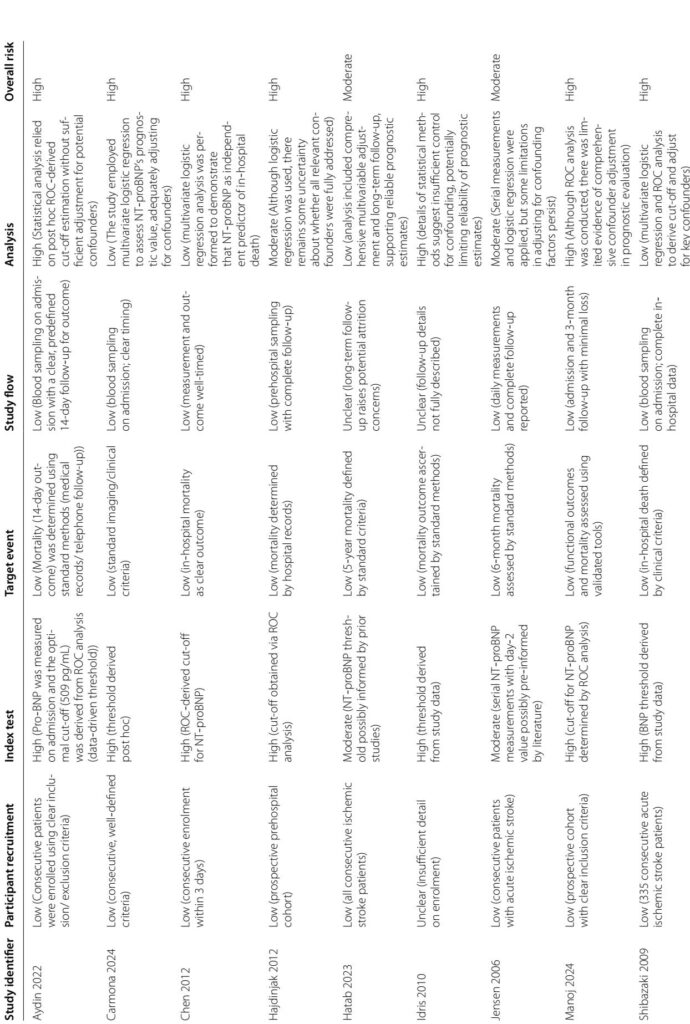
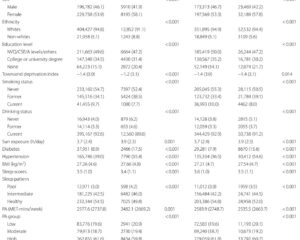
This meta-analysis incorporated data from 11 prospective observational studies, encompassing 2994 patients with confirmed acute ischemic stroke, extracted from five major medical databases up to February 2025. Inclusion criteria required documented NT-proBNP or BNP measurement during the acute or subacute phase and mortality outcomes, either in-hospital or up to three months post-event. Diagnostic accuracy metrics—sensitivity, specificity, likelihood ratios, diagnostic odds ratio, and area under the receiver operating characteristic curve (AUROC)—were pooled using a bivariate random-effects model. Risk of bias was assessed through the QUAPAS tool, and evidence certainty graded by GRADE methodology.
Key Findings
The pooled NT-proBNP demonstrated strong prognostic performance for mortality prediction in ischemic stroke. The overall sensitivity was 0.83 (95% CI 0.73–0.89), and specificity was 0.77 (95% CI 0.67–0.84), with an AUROC of 0.87 indicating good discriminative ability. Subgroup analyses revealed that NT-proBNP predicted in-hospital mortality with 84% sensitivity and 70% specificity (AUROC 0.86), while 3-month mortality prediction had 81% sensitivity and 87% specificity (AUROC 0.91). The positive likelihood ratio (3.5) and negative likelihood ratio (0.23) corresponded to a diagnostic odds ratio of 16, reflecting meaningful shifts in posttest probabilities.
Heterogeneity between studies was significant, influenced primarily by patient age and sample size rather than NT-proBNP cut-off thresholds or follow-up duration. The risk of bias was high in most studies due to post hoc determination of biomarker thresholds and limited adjustment for confounders. Nevertheless, the collective evidence supports the robustness of NT-proBNP as a prognostic marker.
Expert Commentary
NT-proBNP integrates cardiac and cerebrovascular pathology, serving as a surrogate for the cardiocerebral axis dysfunction common in ischemic stroke. Elevated levels may indicate occult cardiac disease or systemic stress responses that exacerbate neurological injury. This biomarker’s moderate-to-high sensitivity and specificity, especially in predicting early mortality, advocate for its incorporation into stroke risk stratification frameworks.
However, limitations exist, including the heterogeneity of cut-off values and patient characteristics, and reliance on observational data with potential confounding. Standardization of measurement protocols and prospective validation in well-defined cohorts are essential before routine implementation. Additionally, combining NT-proBNP with clinical scores and other biomarkers might enhance predictive accuracy.
Conclusions
NT-proBNP is a promising biomarker with moderate-to-high accuracy in predicting mortality among ischemic stroke patients, both during hospitalization and at three months post-stroke. Its use can substantially refine risk stratification, guide intensified monitoring, and inform therapeutic decision-making. Future multicenter prospective studies should aim to establish standardized cut-off values and assess the impact of NT-proBNP-guided clinical interventions on patient outcomes.
References
1. Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018;38:208–11.
2. Campbell BCV et al. Ischaemic stroke. Nat Rev Dis Primers. 2019;5:70.
3. Saceleanu VM et al. Integrative approaches in acute ischemic stroke. Biomedicines. 2023;11:2617.
4. Harpaz D et al. B-type natriuretic peptide as a biomarker for stroke triaging. Biosensors. 2020;10:107.
5. Cao Z et al. BNP and NT-proBNP as diagnostic biomarkers. Int J Mol Sci. 2019;20:1820.
6. Liu HH et al. Prognostic value of NT-proBNP in chronic coronary syndrome. Cardiovasc Diabetol. 2021;20:84.
7. Cushman M et al. NT-proBNP and stroke risk. Stroke. 2014;45:1646–50.
8. Chen Z et al. Brain-heart interaction after stroke. Circ Res. 2017;121:451–68.
9. Zeng QL et al. NT-proBNP correlates with prognosis in neurological patients. Ann Transl Med. 2021;9:28.
10. Mouzarou A et al. NT-proBNP in hypertensive heart disease. Diagnostics. 2025;15:113.
11. García-Berrocoso T et al. B-type natriuretic peptides and mortality after stroke. Neurology. 2013;81:1976–85.