Highlight
1. Patients with acute basilar artery occlusion (BAO) selected for EVT by noncontrast CT (NCCT) have similar 90-day functional outcomes and safety profiles compared to those selected by CT perfusion (CTP).
2. In late-window EVT (6-24 hours post-onset) for anterior circulation large vessel occlusions, penumbra volume on CTP significantly modifies treatment benefit, whereas core volume and mismatch ratio do not.
3. Meta-analysis across acute ischemic stroke patients shows no significant difference in functional independence between NCCT-based and CTP-based selection for EVT; however, CTP selection is associated with lower mortality during follow-up.
4. NCCT-based selection may favor patients with large core infarcts regarding functional outcomes.
Study Background and Disease Burden
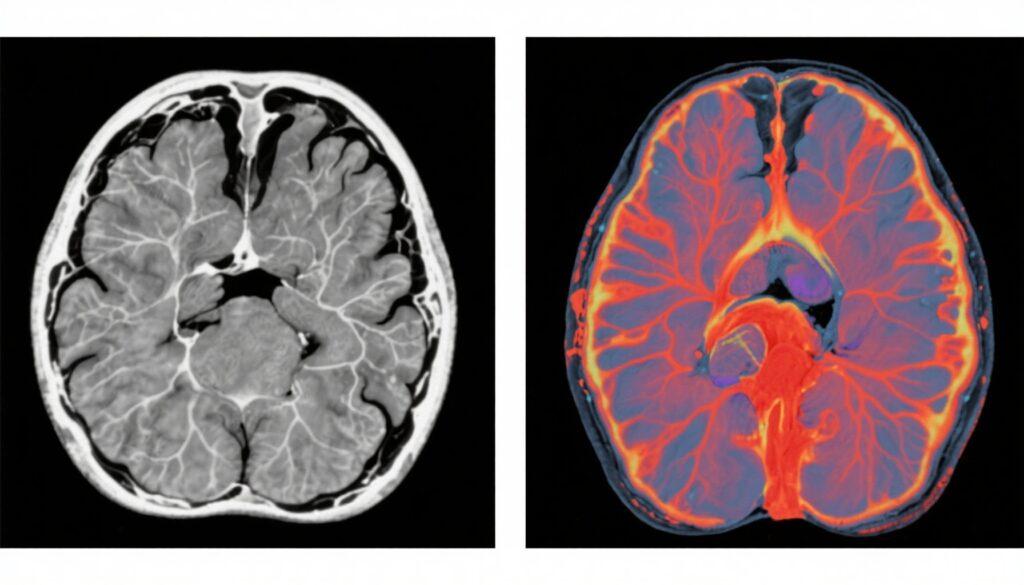
Stroke remains a leading cause of morbidity and mortality worldwide, with rapid identification and treatment of large vessel occlusions pivotal for improved outcomes. Endovascular therapy (EVT) has revolutionized acute ischemic stroke management, especially within early and late time windows. Imaging selection criteria are critical to identify patients likely to benefit from EVT, traditionally relying on advanced modalities such as CT perfusion (CTP) or MRI perfusion/diffusion imaging to delineate ischemic core and penumbra.
However, CTP and MRI are not uniformly accessible, especially in resource-limited settings. Noncontrast computed tomography (NCCT) and CT angiography (CTA) remain widely available and rapid tools to assess stroke patients and vascular occlusion. Understanding whether NCCT alone suffices for patient selection or if CTP provides important incremental prognostic or therapeutic value has significant implications for clinical workflow and health equity.
Study Designs
This analysis synthesizes findings from three key studies:
1. The ATTENTION and ATTENTION IA trials post hoc analysis evaluated 406 patients with acute basilar artery occlusion (BAO) within 24 hours of onset, comparing functional and safety outcomes between patients selected by NCCT versus CTP for EVT.
2. The MR CLEAN-LATE secondary analysis focused on patients with anterior circulation large vessel occlusions presenting in the late window (6-24 hours) selected by collateral status on CTA, with correlated assessment of CTP parameters (core, penumbra, mismatch) and their interaction with EVT effect.
3. A systematic review and meta-analysis encompassing 16 studies (12,199 patients) compared NCCT (±CTA) versus CTP imaging for EVT selection in acute ischemic stroke, analyzing functional outcomes, thrombolysis success, hemorrhagic complications, and mortality.
Key Findings
1. ATTENTION and ATTENTION IA Trials:
– Among 406 eligible BAO patients, 67.5% were selected by NCCT, 32.5% by CTP.
– Median baseline NIHSS was high (23), reflecting severe deficits; median pc-ASPECTS was 9, indicating moderate infarct extent.
– No significant difference in the primary outcome (90-day modified Rankin Scale [mRS] 0-3) between NCCT and CTP groups (48.5% vs 45.5%, p=0.56).
– Secondary outcomes including functional independence (mRS 0-2), symptomatic intracranial hemorrhage, and 90-day mortality were also similar.
– IPTW-adjusted odds ratio for favorable outcome showed no difference (OR 0.88, 95% CI 0.58-1.32).
– These results suggest NCCT-based selection is non-inferior to CTP in BAO within the 24-hour window.
2. MR CLEAN-LATE Secondary Analysis:
– Included 313 patients with late-window anterior circulation occlusion and available CTP data.
– EVT beneficially associated with outcome, but this effect was strongly modified by penumbra volume (p<0.001).
– Patients with large penumbra volumes (≥120 mL) had markedly greater EVT treatment effects (adjusted common OR 6.89).
– Conversely, smaller penumbra volumes (≤72 mL) showed a trend toward harm with EVT.
– Core volume and mismatch ratio exhibited no significant effect modification.
– This suggests penumbra volume on CTP is a critical biomarker for EVT benefit in late-window ischemic stroke.
3. Systematic Review and Meta-Analysis:
– No significant difference in functional independence (mRS 0-2) between patients selected with NCCT±CTA or CTP (OR 1.09, 95% CI 0.98-1.21).
– Safety outcomes including symptomatic intracranial hemorrhage and reperfusion (TICI 2b/3) were comparable.
– Significantly lower odds of death during follow-up were observed with CTP selection compared to NCCT (OR 0.78, 95% CI 0.70-0.88).
– Notably, NCCT selection favored better outcomes in patients with large core infarcts.
– Risk of bias was identified in several observational and post hoc studies, cautioning interpretation.
Comparative Analysis
The ATTENTION trials’ head-to-head comparison in BAO patients showed functional equivalence and safety between NCCT and CTP in selecting patients for EVT. This finding is clinically impactful because BAO is a severe stroke subtype with limited advanced imaging availability.
The MR CLEAN-LATE results contextualize the nuanced role of CTP parameters in late-window anterior circulation strokes, highlighting the importance of penumbra volume over core or mismatch for identifying EVT responders. This suggests that CTP remains valuable for refining patient selection in specific clinical scenarios.
The meta-analysis provides a broader perspective across acute ischemic strokes, reinforcing the general equivalence of NCCT and CTP selection strategies for functional outcomes but suggesting potential mortality advantages with CTP selection. The better functional outcomes in NCCT-selected large-core patients challenge the convention that perfusion imaging is always superior.
Expert Commentary
Contemporary stroke management requires balancing precision imaging with timely treatment access. These data support that in centers lacking routine CTP, NCCT-based algorithms remain appropriate, especially for BAO within 24 hours. Nonetheless, in late-window anterior circulation strokes, CTP’s ability to delineate penumbra may optimize patient benefit-risk assessment.
Limitations include post hoc analyses, potential confounders despite statistical adjustments, and varying imaging protocols across studies. Further prospective randomized trials are needed to confirm these findings and refine imaging paradigms.
Conclusion
Recent evidence indicates that noncontrast CT with or without CT angiography is a valid and practical imaging modality for selecting patients with acute ischemic stroke, including basilar artery occlusion, for endovascular therapy. CT perfusion adds incremental value in late-window cases by identifying critical penumbra volumes predictive of treatment benefit. Overall, imaging selection should be tailored to patient presentation, stroke subtype, and available resources, striving for rapid treatment to maximize outcomes.
References
1. Hu W, Nguyen TN, et al. Noncontrast CT vs CT Perfusion Imaging in Patients With Basilar Artery Occlusion: Analysis of the ATTENTION and ATTENTION IA Trials. Neurology. 2025;105(3):e213911.
2. Olthuis SGH, Pinckaers FME, et al. CT Perfusion Imaging After Selection for Late-Window Endovascular Stroke Treatment: Secondary Analysis of the MR CLEAN-LATE Randomized Trial. JAMA Neurol. 2025;82(6):589-596.
3. Zhang Y, Zhao Y, et al. Selection by Noncontrast Computed Tomography With or Without Computed Tomography Angiography Versus Computed Tomography Perfusion for Endovascular Therapy in Patients With Acute Ischemic Stroke: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2025;14(12):e038173.