Background
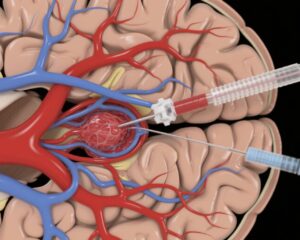
Persistent upper extremity (UE) impairment following a stroke is a prevalent condition affecting many individuals. People recovering from chronic ischemic stroke require durable treatment options that can foster significant improvements in their rehabilitation journey. This report aims to evaluate the long-term effects of vagus nerve stimulation (VNS) when paired with rehabilitation programs aimed at enhancing motor function, activity levels, and overall participation in daily life for individuals experiencing upper extremity impairment after ischemic stroke.
Methods
The analysis presented in this report is a post hoc evaluation of data from the VNS-REHAB randomized clinical trial, which is designed to assess the efficacy of vagus nerve stimulation during rehabilitation to improve upper limb motor functionality post-stroke. Initially, the study engaged 108 participants across 19 medical sites diagnosed with chronic ischemic stroke and moderate-to-severe upper extremity impairment. Participants underwent 18 sessions of intensive, task-specific rehabilitation within a clinical setting, followed by three months of self-directed exercise at home, utilizing either active (real) or sham (control) vagus nerve stimulation.
After the initial phase, participants who received sham stimulation transitioned to real stimulation alongside continued therapy sessions. All participants dedicated a year to home-based exercises complemented by self-initiated active stimulation. Assessment of outcomes such as the Fugl-Meyer Assessment for upper extremity function, the Wolf Motor Function Test, and various participation metrics occurred at several intervals, culminating at the twelve-month mark.
Results
Of the initial participants, seventy-four individuals (which accounts for 69% of the cohort; 51 males) successfully completed the 1-year follow-up. Their mean age was approximately 59.6 years. Upon analyzing their pooled data, significant improvements were noted at the one-year mark compared to baseline measures across multiple domains. These included:
– **Impairment** as measured by the Fugl-Meyer Assessment for upper extremities: a mean improvement of 5.23 (95% CI, 4.08-6.39; P<0.001).
– **Activity** enhancement measured by the Wolf Motor Function Test yielded a 0.50 increase (95% CI, 0.41-0.59; P<0.001).
– Improved **patient-reported outcomes** included:
– Motor Activity Log-Quality of Movement showed a 0.64 rise (95% CI, 0.46-0.82; P<0.001).
– Motor Activity Log-Amount of Use equally improved by 0.64 (95% CI, 0.46-0.82; P<0.001).
– The Stroke Impact Scale regarding Activities of Daily Living noted a 7.43 rise (95% CI, 5.09-9.77; P<0.001).
– The hand component of the Stroke Impact Scale indicated a significant gain of 17.89 (95% CI, 14.16-21.63; P<0.001).
– The EQ-5D scale demonstrated a mean improvement of 5.76 (95% CI, 2.08-9.45; P<0.05).
– Stroke-Specific Quality of Life noted an enhancement of 0.29 (95% CI, 0.19-0.39; P<0.001).
Conclusions
Participants who underwent treatment involving paired vagus nerve stimulation exhibited sustained improvements across various metrics assessing upper extremity impairment, activity levels, participation, and overall quality of life at the one-year follow-up. Vagus nerve stimulation, which is recognized and approved as a beneficial treatment option by the Food and Drug Administration, presents significant promise for achieving long-lasting benefit in individuals facing chronic upper extremity limitations following ischemic stroke.
Registration
For further details, refer to the registration at the following URL: [Clinical Trials](https://www.clinicaltrials.gov); Unique identifier: NCT03131960.
Reference
Kimberley TJ, Cramer SC, Wolf SL, Liu C, Gochyyev P, Dawson J; VNS-REHAB Trial Group. Long-Term Outcomes of Vagus Nerve Stimulation Paired With Upper Extremity Rehabilitation After Stroke. Stroke. 2025 Aug;56(8):2255-2265. doi: 10.1161/STROKEAHA.124.050479. Epub 2025 May 7. PMID: 40329913.