Highlight
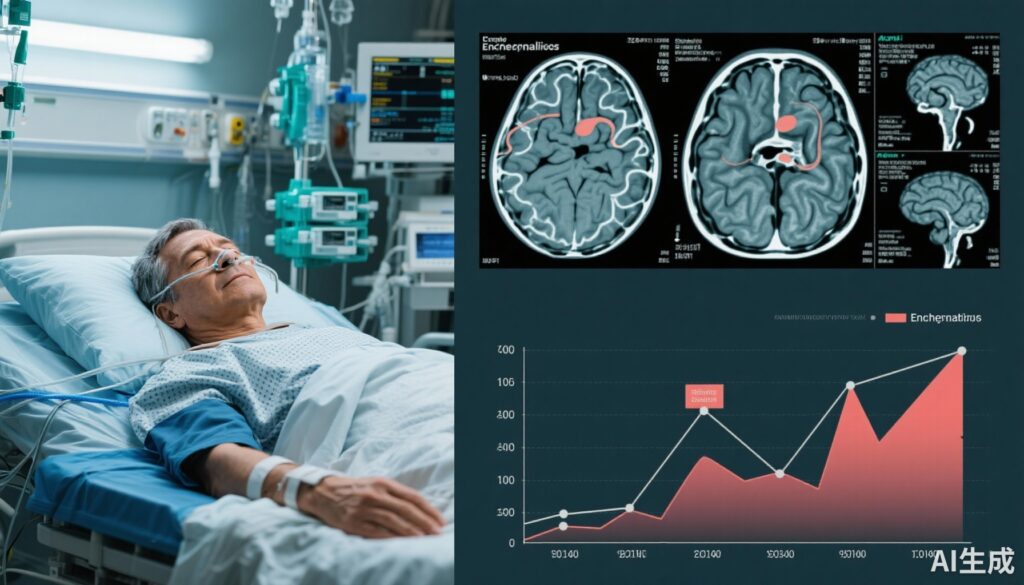
– Approximately half of critically ill adult patients with acute encephalitis experience moderate to severe disability or death at 3 months post-ICU admission.
– Autoimmune encephalitis patients demonstrate significant functional improvement through 1 year, unlike other etiologic groups.
– Advanced age and immunocompromised status independently predict unfavorable outcomes, while early intravenous acyclovir correlates with improved prognosis.
– Functional independence remains largely stable beyond 3 months, underscoring the critical window for early intervention and rehabilitation.
Study Background and Disease Burden
Acute encephalitis is a severe neurologic syndrome characterized by brain inflammation leading to cognitive impairment, seizures, and potential death. Despite advances in diagnosis and critical care, outcomes remain highly variable and often poor, particularly in severe presentations requiring intensive care unit (ICU) admission. The global disease burden is significant, with high morbidity and mortality rates, yet long-term functional trajectories following severe encephalitis are poorly characterized. Understanding the patterns and predictors of recovery across different etiologies—infectious, autoimmune, and others—can inform prognosis, therapeutic strategies, and rehabilitation resources. This knowledge gap motivated the ENCEPHALITICA multicenter cohort study in France, providing a rigorous prospective assessment of functional outcomes and recovery trajectories in adults critically ill with acute encephalitis.
Study Design
This prospective observational cohort study was conducted between October 2017 and April 2021 across 31 French centers specializing in critical care and neurology. It included 310 adult patients with probable or confirmed acute encephalitis based on clinical and cerebrospinal fluid (CSF) criteria who required ICU management. Encephalitis causes were classified into four groups: infectious (including viral and bacterial), autoimmune, other specified causes, and unknown origin. Baseline demographics, clinical features, immunocompromised status, and treatments—including antiviral therapy—were prospectively collected. The primary endpoint was an unfavorable functional outcome at 3 months, defined as a modified Rankin Scale (mRS) score of 3 to 6, indicating moderate to severe disability or death. Secondary outcomes included recovery trajectories assessed by mRS through one year post-admission. Data analysis spanned from May 2023 to June 2025.
Key Findings
Among the cohort (median age 60 years, 57.1% male), infectious encephalitis accounted for 39.7%, autoimmune 13.5%, other causes 11.9%, and 34.8% remained of unknown etiology. At 3 months, 51.9% (95% CI, 46.2%-57.6%) exhibited an unfavorable outcome, including a mortality rate of 27.1%. Key factors associated with poor outcome were older age (adjusted OR 1.28 per 5-year increment, 95% CI 1.16–1.41) and immunocompromised status (OR 3.12, 95% CI 1.57–6.40). Importantly, administration of intravenous acyclovir on ICU admission day was linked with lower risk of unfavorable outcome (OR 0.38, 95% CI 0.20–0.72), affirming the benefit of prompt antiviral therapy.
Functional independence assessed by mRS remained stable from 3 months to 1 year (difference in proportions 1.1%; 95% CI, -6.9% to 9.2%), indicating limited late recovery when considering the entire cohort. However, stratification by encephalitis etiology revealed that patients with autoimmune encephalitis experienced significant improvement during this period (difference in proportions 8.9%; 95% CI, 1.2% to 16.6%), suggesting ongoing recovery potential. No statistically significant late improvements were observed in infectious, other, or unknown origin groups.
These findings are clinically relevant as they highlight differing natural history trajectories based on encephalitis cause and emphasize the critical importance of etiological diagnosis for prognostication and targeted management planning.
Expert Commentary
This study by Sonneville et al. represents a landmark investigation of functional outcomes after severe encephalitis in the ICU setting, leveraging a robust multicenter prospective design and large sample size. The high rate of unfavorable outcomes and mortality underscores the gravity of encephalitis-related critical illness but also reveals a positive prognostic subgroup—autoimmune encephalitis patients—who exhibit progressive functional recovery up to one year. This aligns with emerging literature underscoring the reversibility of immune-mediated encephalopathies with appropriate immunotherapy and rehabilitation.
The independent association of aged and immunocompromised status with poor outcomes corroborates prior studies demonstrating vulnerability in these populations. Early intravenous acyclovir’s favorable correlation supports current clinical guidelines advocating prompt empiric antiviral treatment in suspected viral encephalitis, particularly herpes simplex virus, the most common treatable cause.
Limitations include potential residual confounding, classification challenges for encephalitis etiology, and absence of detailed neuroimaging or biomarker data to correlate with functional trajectories. Additionally, the generalizability beyond French academic centers warrants caution but the multicenter scope enhances external validity.
Overall, this study advances understanding of long-term recovery in encephalitis and strengthens a framework for individualized prognosis and management.
Conclusion
This comprehensive multicenter cohort study elucidates functional outcomes and recovery trajectories among adults with severe encephalitis requiring ICU care. Half of patients experience moderate to severe disability or death at 3 months, with age and immunocompromised status as key adverse prognostic factors. Timely initiation of intravenous acyclovir confers a survival benefit. Notably, patients with autoimmune encephalitis exhibit significant functional improvement through one year, contrasting with other etiologies. These findings advocate for early etiological diagnosis and tailored longitudinal support including rehabilitation to optimize recovery. Future research should integrate biomarker and imaging correlates, and explore interventions that enhance neuroplasticity and functional restitution.