Highlight
- Schizophrenia is associated with reduced non-neuromelanin-bound brain iron in the substantia nigra and ventral tegmental area (SN-VTA).
- Lower magnetic susceptibility indicating decreased iron correlates with elevated striatal dopamine synthesis measured by [18F]-DOPA PET.
- These findings support a mechanistic link between brain iron deficiency and hyperdopaminergia in schizophrenia pathology, particularly in early-course patients.
- The study leveraged quantitative susceptibility mapping (QSM) MRI, neuromelanin-sensitive MRI (NM-MRI), diffusion tensor imaging (DTI), and PET to dissect iron, neuromelanin, and myelin contributions.
Study Background
Schizophrenia is a severe psychiatric disorder characterized by complex neurochemical alterations, including dysregulated dopamine neurotransmission, particularly elevated dopamine synthesis in the striatum. Dopaminergic hyperactivity contributes to positive symptoms such as hallucinations and delusions. Parallel neuroimaging studies have reported reduced brain iron in schizophrenia, yet the mechanistic relationship between brain iron and dopamine dysregulation remains poorly understood. Preclinical evidence implicates midbrain iron deficiency as a driver of striatal hyperdopaminergia, suggesting iron may play a modulatory role in dopamine synthesis and release.
Iron is critical for dopamine metabolism as a cofactor for tyrosine hydroxylase, the rate-limiting enzyme in dopamine synthesis. Additionally, iron influences myelination and neuronal integrity, and its imbalance may impact neurodevelopment and neurochemical regulation relevant to schizophrenia pathophysiology.
Study Design
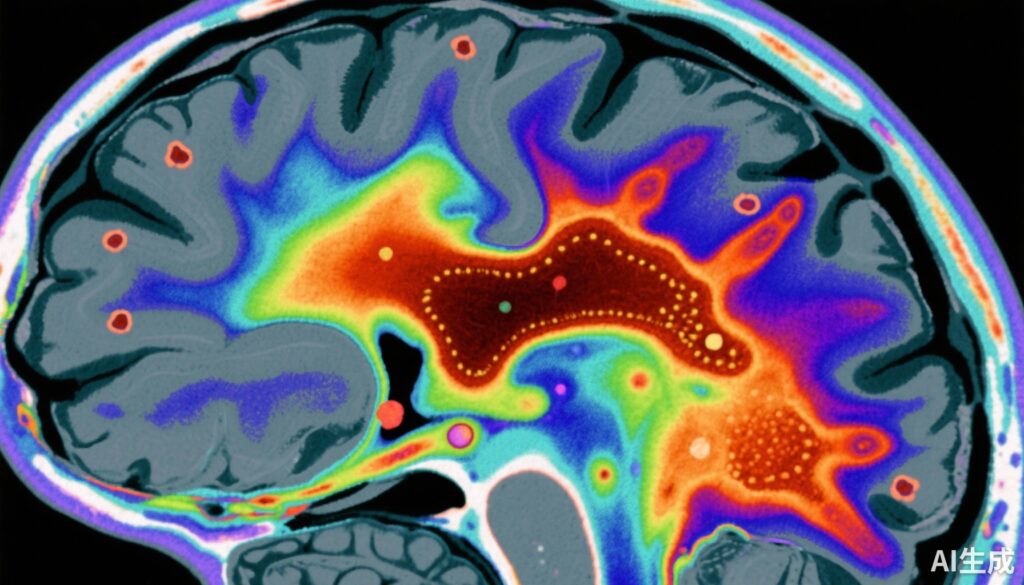
This case-control study conducted by Vano et al. included 159 participants: 79 patients with early-course schizophrenia (including antipsychotic-naïve or antipsychotic-free individuals) and 80 healthy controls. Quantitative susceptibility mapping (QSM) MRI was utilized to quantify magnetic susceptibility—a proxy for brain iron—in the substantia nigra and ventral tegmental area (SN-VTA).
Since magnetic susceptibility signals can be influenced by neuromelanin and myelin, neuromelanin-sensitive MRI (NM-MRI) and diffusion tensor imaging (DTI) were employed in a subset of 99 participants (61 schizophrenia patients, 38 controls) to control for these confounding factors. NM-MRI assessed neuromelanin contrast, while DTI measured mean diffusivity, inversely related to myelin content.
In a further subset of 40 schizophrenia patients, dopamine synthesis capacity was assessed using [18F]-DOPA positron emission tomography (PET), providing the kinetic parameter Ki cer as a quantitative measure of striatal dopamine synthesis.
Key Findings
The study found a statistically significant reduction in magnetic susceptibility in the SN-VTA region in schizophrenia patients compared to controls, with an effect size (Cohen’s d) of -0.66 (95% CI, -0.98 to -0.34). This suggests lower brain iron concentration in this critical midbrain dopaminergic region.
Importantly, the reduction in QSM-derived magnetic susceptibility persisted after statistically adjusting for neuromelanin NM-MRI contrast and DTI mean diffusivity, indicating that the iron deficiency was not confounded by changes in neuromelanin or myelin content.
Correlation analysis demonstrated a significant inverse relationship (r = -0.44) between SN-VTA magnetic susceptibility and striatal dopamine synthesis capacity (Ki cer) assessed by PET. Thus, individuals with lower brain iron exhibited higher dopamine synthesis in the striatum, supporting the hypothesis that brain iron deficiency may promote hyperdopaminergia.
Regional analysis indicated the ventral SN-VTA exhibited the strongest associations, highlighting this subregion’s particular relevance to dopamine dysregulation in schizophrenia.
Expert Commentary
The integration of multimodal imaging techniques in this large cohort represents a rigorous approach to deciphering the neurochemical underpinnings of schizophrenia. By isolating the contribution of non-neuromelanin-bound brain iron and confirming its association with dopamine synthesis, the study advances our understanding beyond correlational findings to suggest a mechanistic link that complements extant dopaminergic models.
While antipsychotic treatment can affect brain iron and dopamine parameters, the inclusion of antipsychotic-naïve or off medication participants strengthens the argument that these findings reflect intrinsic disease pathology rather than medication effects.
Limitations include the cross-sectional design precluding causal inference and the modest subsample size for PET imaging. Longitudinal studies are needed to elucidate whether brain iron deficits contribute to illness progression or treatment response. Additionally, the biological mechanisms by which iron deficiency elevates dopamine synthesis—potentially through enzyme cofactor availability or oxidative stress alterations—require further molecular investigation.
These findings also open intriguing therapeutic possibilities. Iron supplementation or agents targeting iron metabolism in the brain might modulate dopaminergic dysfunction and improve clinical outcomes, warranting careful clinical trials.
Conclusion
This seminal study provides compelling evidence that lower non-neuromelanin-bound iron in the substantia nigra and ventral tegmental area is linked to striatal dopamine hyperactivity in early-course schizophrenia. This novel insight into schizophrenia neurobiology highlights brain iron as a critical factor influencing dopamine synthesis and potentially symptomatology.
Future research should focus on validating these findings longitudinally, exploring mechanistic pathways, and translating them into targeted therapies that address iron metabolism abnormalities. Such advances could enhance personalized treatment paradigms and potentially mitigate dopaminergic dysregulation in schizophrenia.
Funding and Clinical Trials Registration
The study was funded by institutions and grants as specified in the original publication. No clinical trial registration was indicated for this imaging study.
References
Vano LJ, McCutcheon RA, Sedlacik J, et al. Reduced Brain Iron and Striatal Hyperdopaminergia in Schizophrenia: A Quantitative Susceptibility Mapping MRI and PET Study. Am J Psychiatry. 2025;182(9):830-839. doi:10.1176/appi.ajp.20240512.