Highlight
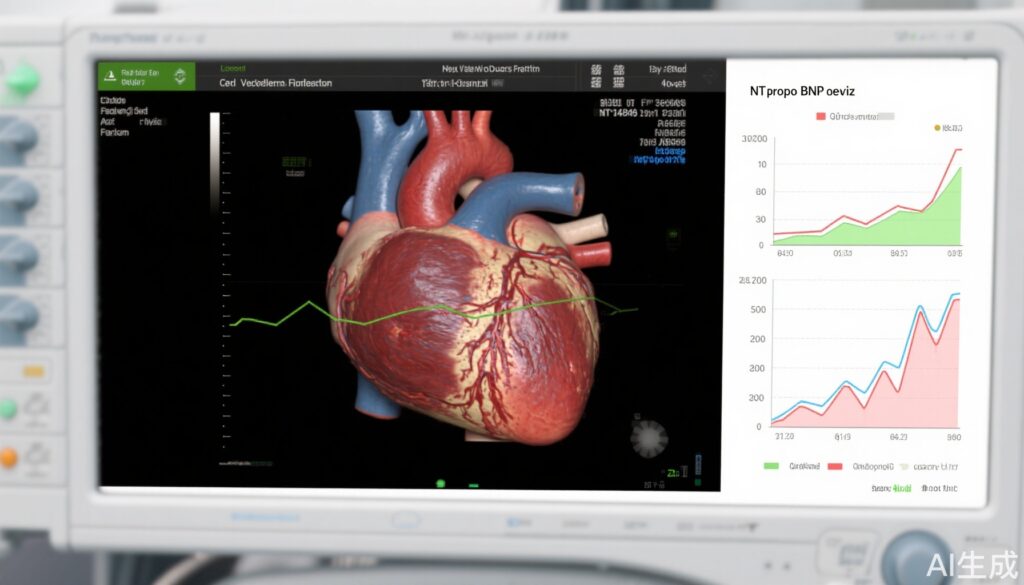
- Sacubitril/valsartan (sac/val) significantly reduces NT-proBNP levels compared with valsartan (val) in patients with LVEF >40% and worsening heart failure (WHF).
- This NT-proBNP-lowering effect of sac/val is consistent across patients with different degrees of structural abnormalities, including left ventricular hypertrophy (LVH) and left atrial enlargement (LAE).
- No significant difference in cardiovascular efficacy endpoints was observed based on structural abnormality status.
- Patients with both LVH and LAE had higher odds of hyperkalemia when treated with sac/val, indicating a need for close monitoring.
Study Background and Disease Burden
Heart failure (HF) with mildly reduced or preserved ejection fraction (LVEF >40%) constitutes a significant portion of HF patients and is associated with substantial morbidity and mortality. Despite clinical advances, treatment options for this population remain limited, especially in the context of worsening heart failure (WHF). Sacubitril/valsartan, a combined angiotensin receptor-neprilysin inhibitor, has shown benefit in HF with reduced ejection fraction, but its role and mechanisms in patients with preserved or mildly reduced LVEF are less well understood.
Structural cardiac abnormalities such as left ventricular hypertrophy (LVH) and left atrial enlargement (LAE) commonly accompany HF and are markers of disease severity and remodeling. These changes can influence neurohormonal activation and cardiac biomarker profiles, potentially modifying therapeutic response.
The PARAGLIDE-HF trial previously demonstrated that sacubitril/valsartan significantly reduces NT-proBNP compared with valsartan alone in patients with LVEF >40% and worsening HF. However, the impact of structural abnormalities—specifically LVH and LAE—on the efficacy and safety of sacubitril/valsartan in this population remained undefined, necessitating this subanalysis.
Study Design
The PARAGLIDE-HF trial enrolled patients with LVEF >40% experiencing recent WHF. Patients were stratified into three groups based on echocardiographic assessment of LVH and LAE:
- Both LVH and LAE present
- Either LVH or LAE present
- Neither LVH nor LAE present
The primary efficacy endpoint was the time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8. Secondary endpoints included recurrent cardiovascular composite events such as HF hospitalizations, urgent HF visits, and cardiovascular death. Safety endpoints assessed included symptomatic hypotension, hyperkalemia, and worsening renal function.
Key Findings
Among 466 randomized patients, complete data for LVH and LAE were available in 454 (97.4%). Of these, 157 (34.5%) exhibited both LVH and LAE, 178 (39.2%) had either LVH or LAE, and 119 (26.2%) had neither.
Sacubitril/valsartan consistently produced a greater reduction in NT-proBNP compared with valsartan alone across all structural groups. The interaction test for differential treatment effect by structural abnormality category was not significant (P interaction = 0.705), indicating sac/val efficacy is independent of LVH and LAE status.
Secondary cardiovascular outcomes (recurrent HF-related events and cardiovascular death) showed no significant interaction between treatment response and the degree of structural abnormality.
Safety analysis revealed that patients with both LVH and LAE had a significantly higher likelihood of developing hyperkalemia when treated with sac/val compared to valsartan (odds ratio 2.41, P interaction = 0.024). Incidences of hypotension and worsening renal function did not differ significantly across groups.
Expert Commentary
The analysis from PARAGLIDE-HF provides valuable insight into the management of HF patients with mildly reduced or preserved ejection fraction who have structural cardiac remodeling. The robust NT-proBNP reduction with sac/val regardless of LVH or LAE suggests that neurohormonal modulation conferred by neprilysin inhibition is effective across diverse cardiac substrates.
However, the higher risk of hyperkalemia in patients with combined LVH and LAE warrants caution. This finding aligns with the known pathophysiological interplay between myocardial remodeling, impaired renal handling of potassium, and RAAS blockade. Clinical practitioners should incorporate vigilant potassium monitoring and adjust concomitant medications accordingly.
Limitations include relatively short follow-up for clinical events and lack of detailed tissue characterization. Future studies assessing long-term outcomes and mechanistic biomarkers will enrich understanding.
Conclusion
In patients with LVEF >40% and recent worsening heart failure, sacubitril/valsartan reduces NT-proBNP more effectively than valsartan alone, independent of left ventricular hypertrophy and left atrial enlargement status. No modification of cardiovascular efficacy was detected by degree of structural abnormalities. Nonetheless, patients with both LVH and LAE face increased hyperkalemia risk under sac/val therapy, underscoring the need for individualized safety monitoring.
These findings support the broader applicability of sacubitril/valsartan in HF populations with preserved or mildly reduced ejection fraction and highlight structural cardiac features as important considerations for safety management.
References
Kittipibul V, Cyr DD, Harrington J, Lala A, Fudim M, Ward JH, Sarwat S, Solomon SD, Hernandez AF, Zieroth S, Starling RC, Mentz RJ. Structural abnormalities and effects of sacubitril/valsartan in patients with mildly reduced or preserved ejection fraction and worsening heart failure: The PARAGLIDE-HF trial. Am Heart J. 2025 Nov;289:105-116. doi: 10.1016/j.ahj.2025.05.004. Epub 2025 May 22. PMID: 40412494.