Highlight
- Frailty status measured before hospitalization predicts discharge location among older patients.
- Higher frailty correlates with increased discharge to skilled nursing facilities or home health services.
- Frailty is associated with nearly doubled odds of hospital readmission and elevated 90-day mortality risk.
- Automated frailty assessments at discharge can inform targeted interventions to reduce adverse outcomes.
Study Background and Disease Burden
The aging population is increasing the burden of hospitalizations for older adults globally. Post-hospital outcomes such as readmission and mortality remain significant concerns, influenced by underlying patient vulnerability. Frailty, a clinical syndrome marked by diminished physiological reserve and increased vulnerability to stressors, has emerged as a critical factor affecting health trajectories in older adults. Despite its importance, integrating frailty assessment into routine hospital care and discharge planning has been inconsistent. Understanding how frailty impacts discharge disposition and subsequent health outcomes can guide more personalized care pathways to improve survival and reduce readmission rates in this vulnerable population.
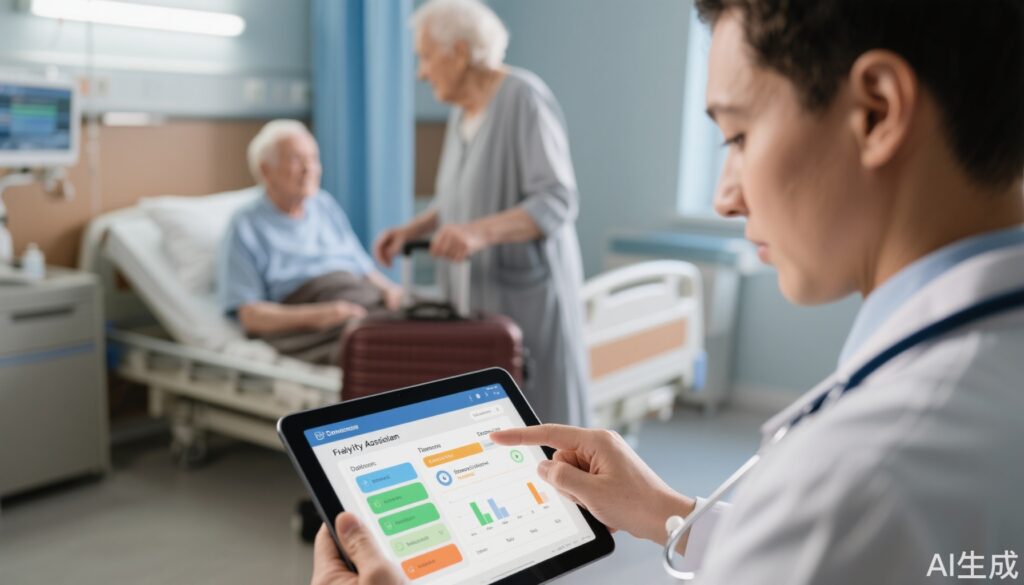
Study Design
This retrospective cohort study analyzed data from over 23,000 patients aged 65 years and older, admitted for at least 24 hours at five hospitals within a US academic health system during 2021 to 2023. The cohort was 53% female. An electronic health record (EHR)-based frailty index was calculated using 54 age-related health deficits documented at the nearest outpatient visit before hospitalization. Patients were categorized into four frailty groups: non-frail, pre-frail, frail, and severely frail. Discharge destinations were classified as home without services, home with home health services, or skilled nursing facilities (SNFs). The primary outcomes were hospital readmission and mortality within 90 days post-discharge.
Key Findings
Among the cohort, 22% were non-frail, 46% pre-frail, 23% frail, and 8% severely frail. Most patients (61%) were discharged home without additional services; 24% went to SNFs, and 15% received home health care.
Patients with frailty had significantly higher likelihoods of discharge to either SNFs or home health care versus home alone. Specifically, adjusted odds ratios (aOR) for discharge to SNFs or home health were 1.20 (95% CI, 1.09–1.33) for frail and 1.17 (95% CI, 1.03–1.34) for severely frail patients.
Importantly, frailty was strongly associated with increased odds of hospital readmission within 90 days— nearly doubling the readmission risk compared to non-frail patients (aOR 1.91; 95% CI, 1.67–2.20). This risk escalated with frailty severity. A similar pattern was seen for mortality post-discharge.
Discharge destination itself influenced mortality: compared to patients discharged directly home, those discharged to SNFs had a more than fivefold increase in mortality (hazard ratio 5.46; 95% CI, 4.43–6.73), while those receiving home health services had a twofold increase (hazard ratio 2.06; 95% CI, 1.54–2.77).
Expert Commentary
The findings underscore the imperative to incorporate frailty screening into hospital discharge planning robustly and systematically. Frailty assessment via electronic health records enables longitudinal and real-time identification of high-risk older adults. Recognizing that the most severely frail patients, especially those discharged to SNFs, face markedly elevated mortality suggests a critical window for enhancing care strategies.
Discharge with home health services for frail patients appears to mitigate some readmission risk, presenting an actionable intervention opportunity. However, the association between SNF discharge and higher mortality invites exploration into care quality, patient selection for SNF care, and additional supportive measures.
Limitations include the retrospective design and the reliance on pre-hospitalization frailty assessment, which may not capture acute illness-related changes. The findings may not generalize to non-academic or non-US settings. Nevertheless, they provide robust, clinically actionable insights into frailty’s prognostic role.
Conclusion
This large-scale cohort study confirms that frailty status is a powerful predictor of discharge disposition, readmission risk, and mortality after hospitalization in older adults. Automated frailty evaluation at discharge allows clinicians to identify vulnerable patients who might benefit most from tailored post-acute care interventions.
Future research should focus on prospective studies integrating frailty-guided discharge protocols and randomized trials assessing interventions such as enhanced home health services to reduce adverse outcomes. Health systems should consider adopting scalable EHR-based frailty assessments to improve transitional care pathways and ultimately patient survival and quality of life after hospital discharge.
References
1. The Association of Frailty With Post-Hospital Discharge Location and Health Outcomes, Journal of the American Geriatrics Society, 2024. https://doi.org/10.1111/jgs.70034
2. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752-762.
3. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was able to ambulate, but now she can’t”. JAMA. 2011;306(16):1782–1793.
4. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3): M146–M156.