Highlight
– In the international, double-blind VESALIUS-CV trial, evolocumab reduced the risk of first major adverse cardiovascular events (3‑point MACE) by 25% versus placebo (HR 0.75; 95% CI 0.65–0.86) over a median 4.6 years.
– Absolute risk reductions were modest: 5‑year Kaplan–Meier estimates were 6.2% with evolocumab vs 8.0% with placebo for 3‑point MACE (absolute risk reduction ~1.8%; NNT ≈56 over 5 years) and 13.4% vs 16.2% for 4‑point MACE (ARR ~2.8%; NNT ≈36).
– No between‑group differences were detected in the incidence of prespecified safety events during follow-up.
Background and disease burden
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of premature morbidity and mortality worldwide. Current secondary‑prevention data show consistent benefit from aggressive low‑density lipoprotein cholesterol (LDL‑C) lowering, including with PCSK9 inhibition, in patients with prior myocardial infarction (MI), ischemic stroke, or symptomatic peripheral artery disease. However, whether PCSK9 inhibition reduces the risk of a first atherosclerotic cardiovascular event among patients who have clinical atherosclerosis or diabetes but no prior MI or stroke has been uncertain. VESALIUS‑CV addresses this evidence gap by evaluating whether evolocumab prevents first major adverse cardiovascular events in this important high‑risk population.
Study design
VESALIUS‑CV was an international, randomized, double‑blind, placebo‑controlled trial (NCT03872401) that enrolled 12,257 patients with either atherosclerosis or diabetes and an LDL‑C of ≥90 mg/dL who had no previous MI or stroke. Participants were randomized 1:1 to evolocumab 140 mg subcutaneously every 2 weeks or matching placebo. The median age was 66 years, 43% were women, 93% were White, and median follow‑up was 4.6 years.
The two prespecified primary efficacy endpoints were: (1) 3‑point MACE (a composite of death from coronary heart disease, myocardial infarction, or ischemic stroke) and (2) 4‑point MACE (3‑point MACE plus ischemia‑driven arterial revascularization). The trial was funded by Amgen and reported in the New England Journal of Medicine (Bohula et al., VESALIUS‑CV Investigators).
Key findings
Primary efficacy results:
– 3‑point MACE occurred in 336 patients in the evolocumab group versus 443 in the placebo group. The 5‑year Kaplan–Meier estimates were 6.2% for evolocumab and 8.0% for placebo.
– The hazard ratio (HR) for the 3‑point MACE primary endpoint was 0.75 (95% CI, 0.65 to 0.86; P < 0.001), corresponding to a 25% relative risk reduction.
– For the 4‑point MACE endpoint, events occurred in 747 patients (evolocumab) versus 907 (placebo). The 5‑year Kaplan–Meier estimates were 13.4% versus 16.2%, respectively. The HR was 0.81 (95% CI, 0.73 to 0.89; P < 0.001), a 19% relative risk reduction.
Absolute benefit and number needed to treat
– Absolute risk reduction (ARR) for 3‑point MACE over 5 years: ~1.8% (8.0% − 6.2%). Estimated NNT ≈ 56 over 5 years.
– ARR for 4‑point MACE over 5 years: ~2.8% (16.2% − 13.4%). Estimated NNT ≈ 36 over 5 years.
These absolute benefits underscore that, although relative risk reductions are clinically meaningful, the population event rates and baseline risk determine the magnitude of absolute benefit.
Safety
The trial report states there was no evidence of a between‑group difference in the incidence of prespecified safety events. Historically, safety concerns associated with PCSK9 inhibitors have included injection‑site reactions, modest effects on glycemia (rare new‑onset diabetes signals), and infrequent neurocognitive complaints; VESALIUS‑CV did not reveal new safety signals over a median 4.6 years. Long‑term surveillance remains important.
Interpretation and clinical implications
VESALIUS‑CV expands the evidence base for PCSK9 inhibition by demonstrating that evolocumab reduces the risk of a first major cardiovascular event in patients with atherosclerosis or diabetes who lack a history of MI or ischemic stroke. The trial addresses a clinical gray zone between primary and secondary prevention: patients who have clinical atherosclerotic disease (for example, peripheral artery disease or coronary atherosclerosis without prior MI) or have diabetes and elevated LDL‑C but have not yet experienced a myocardial infarction or stroke.
Key implications for practice:
- Risk stratification matters. The relative risk reduction (≈25% for 3‑point MACE) is comparable to secondary‑prevention trials, but absolute benefit depends on baseline risk. Higher‑risk patients (for example, multifocal atherosclerosis, poorly controlled diabetes, or markedly elevated LDL‑C despite background therapy) will derive greater absolute benefit and more favorable NNTs.
- LDL‑C lowering strategy. VESALIUS‑CV supports an LDL‑lowering approach that may include PCSK9 inhibition for selected high‑risk patients without prior MI/stroke whose LDL‑C remains elevated. The trial entry threshold was LDL‑C ≥90 mg/dL; clinicians should contextualize this against guideline LDL targets and background lipid‑lowering therapy.
- Cost, access, and patient preference. Although efficacy is clear, cost‑effectiveness analyses and payer policies will influence real‑world uptake. Injectable monthly/biweekly administration and shared decision‑making regarding anticipated absolute benefit are essential.
Strengths and limitations
Strengths:
- Large sample size (12,257 participants), randomized double‑blind design, and clinically meaningful endpoints with long median follow‑up (4.6 years).
- Prespecified dual primary endpoints capturing both hard events and revascularization.
Limitations and considerations:
- Generalizability: 93% of participants were White, limiting inference to more diverse populations. Subgroup analyses by race/ethnicity were not reported in the summary provided.
- Event rates and absolute benefit were modest in the overall cohort; clinicians must identify who among patients without prior MI/stroke are most likely to gain clinically meaningful absolute benefit.
- Industry funding (Amgen) underscores the importance of independent confirmatory analyses and transparent reporting of all safety data.
- Longer follow‑up would clarify effects on total mortality and very long‑term safety.
How this fits with prior evidence and guidelines
Previous randomized trials (e.g., FOURIER) established that evolocumab reduces risk in patients with established atherosclerotic cardiovascular disease. VESALIUS‑CV extends this benefit to selected high‑risk patients without prior MI or stroke, aligning with a pathophysiologic principle that lower LDL‑C reduces atherosclerotic events across risk spectra. Current lipid‑management guidelines endorse LDL‑lowering to risk‑based targets, and VESALIUS‑CV provides randomized outcome data that may inform guideline updates on PCSK9 use in patients who have clinical atherosclerosis or diabetes but no prior major ischemic event.
Conclusion
In VESALIUS‑CV, evolocumab significantly reduced the risk of first major adverse cardiovascular events among patients with atherosclerosis or diabetes without prior MI or stroke, with a 25% relative reduction in 3‑point MACE and no new safety signals over 4.6 years. Absolute benefits were modest on a population level but clinically meaningful for higher‑risk individuals. These results broaden the potential role for PCSK9 inhibition beyond classical secondary prevention, but judicious patient selection, cost considerations, and longer‑term safety and effectiveness data should guide implementation.
Funding and trial registration
Funded by Amgen. VESALIUS‑CV ClinicalTrials.gov number: NCT03872401.
References
1. Bohula EA, Marston NA, Bhatia AK, et al.; VESALIUS‑CV Investigators. Evolocumab in Patients without a Previous Myocardial Infarction or Stroke. N Engl J Med. 2025 Nov 8. doi:10.1056/NEJMoa2514428. PMID: 41211925.
2. Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med. 2017;376:1713‑1722. (FOURIER trial)
3. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC Guideline on the Management of Blood Cholesterol. Circulation. 2019;139:e1082–e1143.
4. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias. Eur Heart J. 2020;41:111‑188.
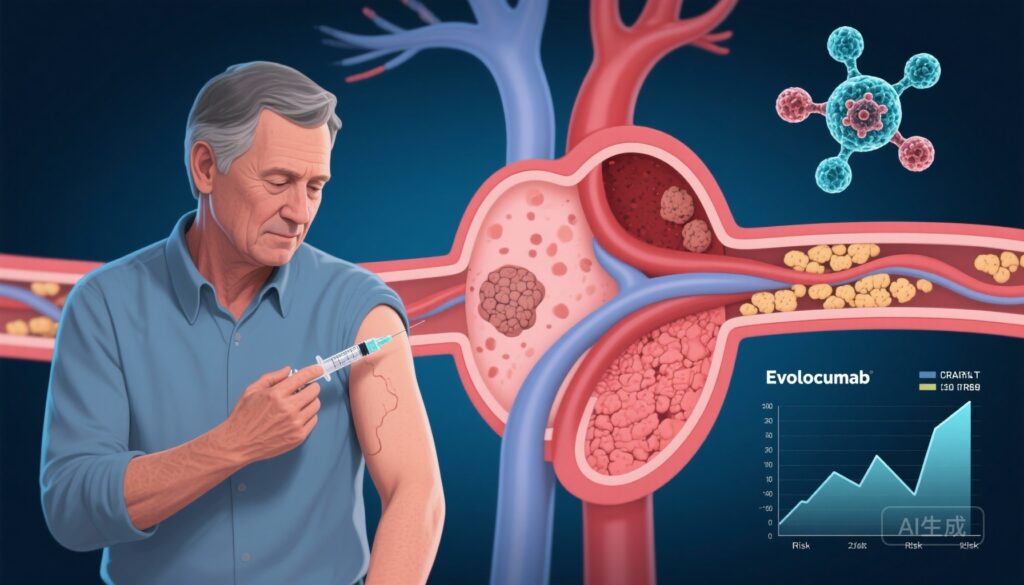
AI image prompt for article thumbnail
A middle‑aged patient in a clinic setting receiving a subcutaneous injection from a healthcare professional; in the background, a semi‑transparent stylized coronary artery with plaque, and overlaid graphs showing descending cardiovascular event curves; clinical trial document and an antibody schematic subtly visible—bright, professional, and evidence‑driven visual tone.