Highlight
– Chronic spinal cord injury (SCI) produces persistent hypotensive complications that are poorly managed with conservative measures despite substantial clinical burden in a cohort of 1,479 participants.
– A purpose-built implantable system using biomimetic epidural electrical stimulation (EES) of the spinal cord produced immediate, robust pressor responses and, in 14 participants, durably reduced severity of hypotensive complications.
– A within-participant, head-to-head comparison showed effective blood pressure regulation required stimulation of the last three thoracic spinal segments rather than lumbosacral targets used for motor recovery.
– Findings support a pathway to a pivotal device trial evaluating safety and efficacy of thoracic-targeted EES for treatment-resistant, underappreciated hypotension after SCI.
Background: the unmet clinical problem
Spinal cord injury disrupts descending autonomic pathways and frequently produces profound cardiovascular dysregulation. Acute and chronic SCI are associated with hypotension, orthostatic intolerance, and episodes of autonomic dysreflexia that together increase morbidity, reduce opportunities for rehabilitation, and degrade quality of life. Hypotension after SCI contributes to reduced cerebral and spinal cord perfusion, which may impair neurological recovery and cognitive function. Despite this high burden, treatment options are limited. Conservative interventions—fluid loading, compression garments, pharmacologic vasopressors—are often only partially effective and can carry side effects that limit adherence and long-term use.
Understanding and treating autonomic cardiovascular dysfunction after SCI is a priority for clinicians and patients. Prior work has shown that spinal neuromodulation can re-enable motor function and also modulate autonomic circuits. However, the spinal segmental targeting and stimulation parameters required to reliably regulate blood pressure have not been fully defined in humans.
Study design and interventions
Phillips et al. (Nat Med 2025) pursued a two-part translational approach. First, they quantified the clinical burden of chronic hypotensive complications in a large cohort of 1,479 participants with SCI to demonstrate unmet need and the limitations of conservative management. Second, they developed and evaluated a dedicated implantable system that delivers biomimetic epidural electrical stimulation (EES) to the spinal cord to restore hemodynamic stability.
Key features of the interventional study:
- Participants: 14 people with chronic SCI and clinically significant hypotensive complications resistant to conservative therapies.
- Device: purpose-built implantable EES system with electrodes positioned epidurally over the spinal cord and a programmable pulse generator capable of customized stimulation patterns intended to mimic physiological sympathetic discharge.
- Comparisons: within-participant head-to-head comparisons of stimulation targeting (last three thoracic segments versus lumbosacral segments) to determine optimal anatomical locus for pressor effects.
- Endpoints: immediate pressor response (acute rise in arterial pressure), durability of hemodynamic improvements (frequency and severity of hypotensive episodes over follow-up), reduction in need for conservative measures, functional and quality-of-life outcomes, and safety/tolerability.
Key findings
The study reported three principal findings: clinical burden of hypotension after SCI, anatomical specificity for effective stimulation, and clinical effectiveness of the implantable system in a small cohort.
1. Burden of chronic hypotensive complications
Analysis of 1,479 participants with SCI established that chronic hypotension and orthostatic intolerance are common and inadequately controlled with standard conservative measures. Many patients remained symptomatic despite use of volume expansion, compression garments, and pharmacologic vasopressors. The authors use these data to motivate the need for new therapeutic strategies targeted specifically at the disrupted spinal autonomic circuits.
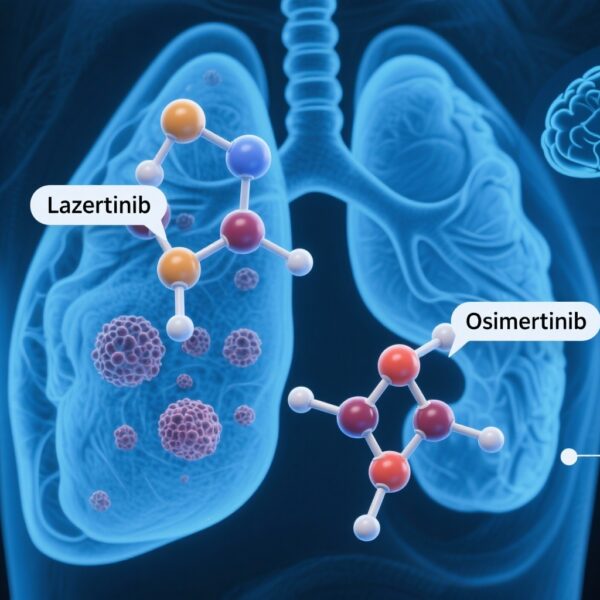
2. Anatomical requirement: last three thoracic segments
A key translational experiment in the study was a within-subject, head-to-head comparison of stimulation of different spinal levels. Epidural stimulation targeting the lowest thoracic segments—the ‘last three thoracic segments’—produced immediate and robust increases in arterial pressure. In contrast, stimulation of the lumbosacral segments (commonly targeted for motor recovery) did not reliably evoke safe or clinically useful pressor responses. These results identify the thoracic spinal cord as the critical locus for recruiting sympathetic preganglionic neurons in the intermediolateral column to increase systemic vascular resistance and venous return.
3. Clinical effectiveness and patient-centered outcomes
In the 14 participants who received the implant, thoracic-targeted EES produced immediate pressor responses during programmed stimulation episodes. Over the reported follow-up, stimulation reduced the severity and frequency of hypotensive complications, decreased reliance on conservative measures (including oral vasopressors and fluid strategies), and improved patient-reported quality of life and capacity for activities of daily living.
Safety and tolerability were acceptable in the cohort reported; the study emphasizes that stimulation parameters and electrode placement must be optimized to avoid unwanted motor activation and to maintain hemodynamic control. The authors present this series as a proof-of-concept that supports a planned larger pivotal device trial to rigorously evaluate safety and efficacy.
Physiological rationale and mechanistic insights
The therapeutic rationale rests on engaging spinal sympathetic outflow below the lesion. Sympathetic preganglionic neurons that regulate arterial tone and venous capacitance are segmentally distributed in the thoracic spinal cord. EES over the lower thoracic segments can recruit these neurons or their afferent inputs to increase sympathetic vasoconstrictor drive, raise systemic vascular resistance, and augment venous return, producing a pressor effect. By contrast, lumbosacral stimulation predominantly engages motor and somatic circuits related to lower-limb function and is less effective at producing the systemic vascular responses needed to correct hypotension.
Expert commentary and limitations
Strengths of the work include its translational design: demonstration of unmet need in a large cohort, development of a purpose-built implantable system, and within-subject anatomical comparisons that directly inform device targeting and programming. The study builds on prior demonstrations that spinal neuromodulation can re-enable lost functions after SCI (for example, targeted neurotechnology for motor recovery) and extends this concept to autonomic control.
However, there are important limitations:
- Small intervention cohort: the implanted-device results derive from 14 participants. While effects were consistent and biologically plausible, the sample size limits precision of effect-size estimates and detection of rarer adverse events.
- Selection and center effects: participants were likely selected for refractory hypotension and ability to undergo implantation and follow-up, which may limit generalizability to broader SCI populations.
- Duration and long-term outcomes: while follow-up in this report shows durable improvements, long-term durability of device efficacy and hardware complications (lead migration, infection, stimulation tolerance) require larger and longer trials.
- Programming complexity and training: optimal stimulation paradigms are individualized and require specialized programming tools and clinician expertise; scalability and access in routine practice will need addressing.
- Comparative effectiveness: head-to-head comparisons versus optimized pharmacologic or combined multimodal strategies were not part of this early series.
Despite these caveats, the results provide a compelling mechanistic and clinical signal supporting a pivotal trial. The findings also have implications for clinical practice if larger studies confirm safety and efficacy: EES could become a targeted option to treat chronic hypotension in people with SCI, thereby improving rehabilitation potential and quality of life.
Clinical implications and practical considerations
For clinicians caring for patients with chronic SCI and refractory hypotension, the study highlights several practical points:
- Careful phenotyping: identify patients whose hypotension is persistent and treatment-resistant, and who might benefit from interventional neuromodulation.
- Targeting matters: epidural electrode placement over the lower thoracic cord is essential to recruit sympathetic circuits—lumbosacral placement is unlikely to remediate hypotension effectively.
- Multidisciplinary care: implantation and follow-up require neurosurgical expertise, autonomic assessment, and structured programming and rehabilitation support.
- Risk–benefit assessment: weigh surgical and device-related risks against the morbidity of chronic hypotension and the limitations of current therapies.
Conclusion and path forward
Phillips et al. report a translationally rigorous, clinically relevant advance: an implantable, thoracic-targeted EES system that can restore hemodynamic stability in people with SCI. By combining a large-scale assessment of clinical burden with mechanistic device development and human testing, the work maps a clear path to a pivotal device trial. If confirmed in larger, controlled studies, this approach could transform management of autonomic cardiovascular dysfunction after SCI, reduce dependence on less effective conservative therapies, and improve rehabilitation engagement and patient-reported outcomes.
Funding and registration
Primary funding sources and trial registration details are provided in the original article: Phillips AA et al., Nat Med. 2025. For trial registration and sponsor information, consult the Nat Med publication and associated ClinicalTrials.gov entries cited therein.
Selected references
1. Phillips AA, Gandhi AP, Hankov N, et al. An implantable system to restore hemodynamic stability after spinal cord injury. Nat Med. 2025 Sep;31(9):2946-2957. doi: 10.1038/s41591-025-03614-w.
2. Wagner FB, Mignardot JB, Le Goff-Mignardot C, et al. Targeted neurotechnology restores walking in humans with spinal cord injury. Nature. 2018;563(7729):65–71.
3. Krassioukov A. Autonomic function following spinal cord injury. Curr Opin Neurol. 2012 Dec;25(6):610-6.
Readers should consult the full Nat Med report for comprehensive methods, participant-level data, and formal trial registration details.