Study Background and Disease Burden
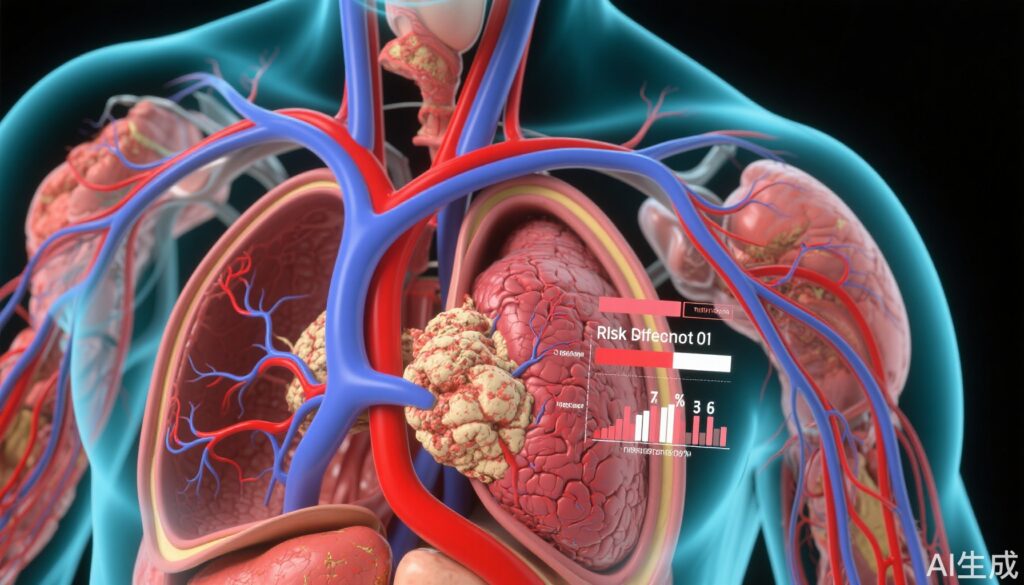
Chest pain is a common clinical presentation that often signals underlying coronary artery disease (CAD), a leading cause of morbidity and mortality worldwide. Stable chest pain evaluation aims to identify patients at risk of myocardial infarction (MI) and death. However, the optimal initial diagnostic strategy remains debated. Coronary computed tomography angiography (CTA) offers a non-invasive visualization of coronary anatomy and plaque burden, potentially allowing better risk stratification than functional testing alone. Despite growing use, whether CTA improves clinical outcomes across all risk groups is unclear. The risk factor weighted clinical likelihood (RF-CL) model estimates patient-specific probability of obstructive CAD by integrating traditional cardiovascular risk factors and symptoms, offering refined pretest risk stratification.
Advancing beyond standard plaque burden assessments, radiomics-based phenotyping characterizes nuanced plaque morphology, potentially improving prediction of myocardial infarction beyond conventional clinical and imaging metrics. The PROMISE and SCOT-HEART trials provide robust data on the prognostic value of coronary CTA and novel radiomic approaches in stable chest pain patients.
Study Design
Two major landmark trials were analyzed:
1. The PROMISE and SCOT-HEART trials randomly assigned 13,748 patients with stable chest pain to initial evaluation with coronary CTA plus usual care or usual care alone (including functional testing). Patients were stratified by RF-CL into very low (≤5%), low (>5% to 15%), and moderate/high (>15%) clinical likelihood of obstructive CAD. The primary endpoint was a composite of myocardial infarction or death at 3 years.
2. A post hoc analysis of coronary CTA images from 1,750 SCOT-HEART patients assessed plaque morphology using radiomic features, integrating eigen radiomic metrics with traditional plaque burden measures. Prognostic associations with fatal or nonfatal MI were evaluated using Cox proportional hazard models and model performance metrics (Harrell’s C-statistic, cumulative dynamic AUC).
Key Findings
PROMISE and SCOT-HEART risk stratification results:
– Overall, 2.3% (313 patients) reached the primary endpoint of MI or death during 3 years.
– Event rates between coronary CTA and usual care groups were broadly similar (risk difference 0.3%, HR 0.84 [95% CI 0.67-1.05]).
– Stratified by RF-CL:
– Very-low and moderate/high likelihood groups showed no significant difference in cardiovascular events between coronary CTA and usual care.
– Patients with low RF-CL who underwent coronary CTA had a statistically significant lower event rate (risk difference 0.7%; HR 0.67 [95% CI 0.47-0.97]).
– The number needed to test (NNT) with CTA to prevent one MI or death within 3 years was 143.
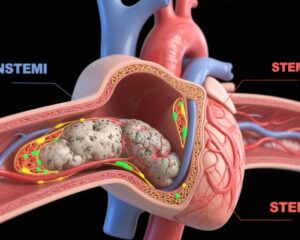
SCOT-HEART radiomic plaque phenotyping:
– Over a median follow-up of 8.6 years, 82 patients suffered fatal or nonfatal MI.
– Fifteen eigen radiomic features were linked with MI in univariate analysis; eight retained significance after adjusting for cardiovascular risk score and plaque burden.
– Adding plaque burden metrics to clinical models yielded modest predictive performance (C-statistic 0.70).
– Incorporating eigen radiomic features significantly elevated model accuracy (C-statistic 0.74), with enhanced predictive value seen from year 5 onwards.
Expert Commentary
These findings reinforce the utility of coronary CTA in the management of stable chest pain, particularly among patients with low but non-negligible risk of CAD. While CTA did not reduce events universally, targeted testing based on RF-CL stratification enhanced prognostic precision and patient outcomes, reducing myocardial infarction or death in the low-likelihood group. The modest NNT suggests efficient resource use in this subgroup.
The innovative use of radiomics to dissect plaque morphology heralds a new era in cardiovascular risk prediction. Beyond simple plaque burden quantification, radiomic phenotyping captures complex textural and morphological features predictive of plaque vulnerability and future events. This precision approach could refine personalized risk stratification and guide tailored preventive strategies.
Limitations include the observational nature of the radiomic analyses, which require prospective validation, and the challenge of integrating complex radiomic data into routine clinical workflows. Nonetheless, these trials provide compelling evidence supporting a paradigm shift toward imaging and computational phenotyping to optimize stable chest pain evaluation.
Conclusions
In summary, coronary CTA combined with risk factor weighted clinical likelihood stratification improves risk prediction and outcomes in patients presenting with new-onset stable chest pain, especially those with low clinical likelihood of obstructive CAD. Advanced radiomic plaque phenotyping further refines long-term myocardial infarction risk beyond traditional clinical and imaging markers. These findings support a more nuanced, personalized diagnostic approach incorporating clinical risk models and sophisticated imaging analytics to better identify patients at risk, improve prognosis, and guide management.
References
Rasmussen LD, Schmidt SE, Knuuti J, Vrints C, Bøttcher M, Foldyna B, Williams MC, Newby DE, Douglas PS, Winther S. Clinical risk prediction, coronary computed tomography angiography, and cardiovascular events in new-onset chest pain: the PROMISE and SCOT-HEART trials. Eur Heart J. 2025 Feb 3;46(5):473-483. doi: 10.1093/eurheartj/ehae742.
Kolossváry M, Lin A, Kwiecinski J, Cadet S, Slomka PJ, Newby DE, Dweck MR, Williams MC, Dey D. Coronary Plaque Radiomic Phenotypes Predict Fatal or Nonfatal Myocardial Infarction: Analysis of the SCOT-HEART Trial. JACC Cardiovasc Imaging. 2025 Mar;18(3):308-319. doi: 10.1016/j.jcmg.2024.08.012.