Introduction and Clinical Context
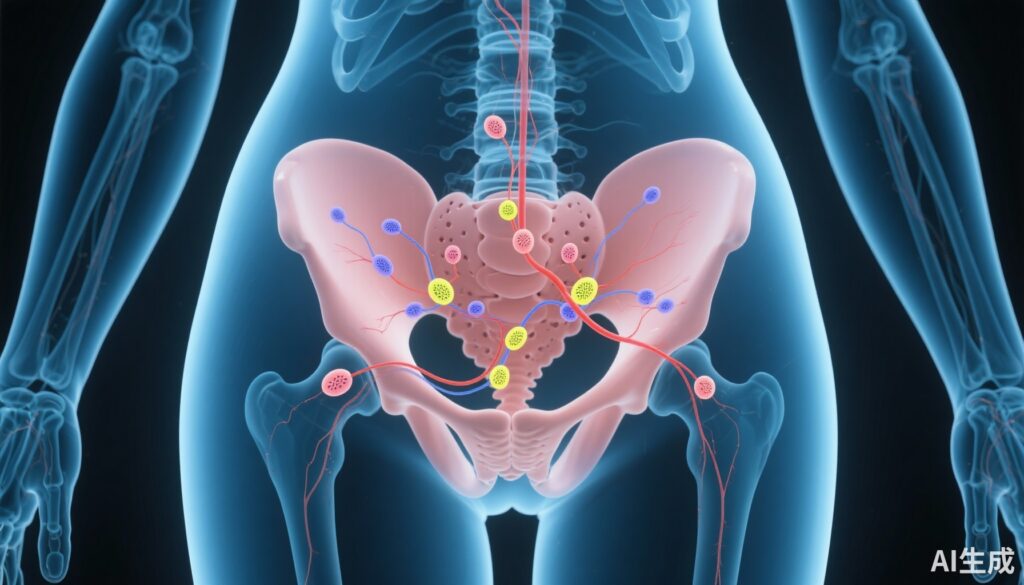
Cervical cancer remains a significant public health challenge worldwide, ranking as the fourth most common cancer among women. Traditionally, management of early-stage cervical cancer includes radical hysterectomy combined with systematic pelvic lymphadenectomy (PLND). This approach allows for accurate staging and regional disease control but is associated with considerable morbidity, including lymphedema, nerve damage, and longer recovery periods.
Recent advances in precision surgical techniques, particularly sentinel lymph node (SLN) biopsy, have revolutionized management in other gynecologic cancers such as endometrial and vulvar cancers. However, the adoption of SLN biopsy in cervical cancer has been cautious, primarily due to concerns over false negatives and the risk of missed metastatic disease.
The SENTIX trial critically evaluates whether SLN biopsy alone, without the comprehensive PLND, can safely be integrated into the standard care for early-stage cervical cancer patients, potentially sparing them from the morbidity of extensive lymphadenectomy.
Study Design and Methodology
The SENTIX trial was a prospective, single-arm, international, noninferiority study that enrolled 731 women with early-stage cervical cancer (stage IA1 with lymphovascular space invasion [LVSI] or stage IB1-IB2 per FIGO 2018). The study spanned from 2016 to 2020 across 47 sites in 18 countries.
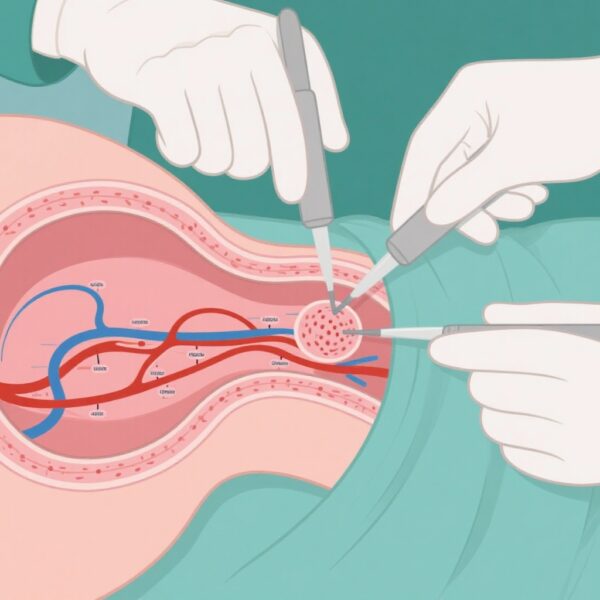
All participants underwent SLN biopsy, followed by hysterectomy or trachelectomy, depending on fertility considerations. The primary intervention was SLN assessment, with ultrastaging for detecting micrometastases, and was followed by systematic pelvic lymph node dissection only if SLNs were undetected, unilateral, or intraoperatively metastatic.
Patients with any of these criteria were excluded from the intention-to-treat cohort. The main endpoints included the 2-year recurrence rate, disease-free survival, and overall survival.
Key Findings and Results
Among 731 enrolled patients, 594 formed the intention-to-treat cohort after applying exclusion criteria. SLN metastases were identified in 82 women (12%), with 56.1% detected intraoperatively and 43.9% by ultrastaging.
Notably, ultrastaging detected N1 disease—metastatic involvement of lymph nodes—in approximately 44% of cases, which would likely have been missed with standard pathological assessment.
At the 2-year follow-up, the recurrence rate was 6.1% (one-sided 95% CI 7.9%), demonstrating noninferiority against a prespecified threshold of 7%. The 2-year disease-free survival was 93.3% (95% CI 91.6%-94.9%), and overall survival was 97.9% (95% CI 97.0%-98.9%).
The data indicate that SLN biopsy without additional PLND does not compromise short-term oncologic outcomes in early-stage disease.
Expert Commentary and Clinical Implications
The SENTIX trial provides robust evidence supporting the safety of omitting systematic pelvic lymphadenectomy when sentinel lymph node biopsy is negative in early-stage cervical cancer. The high detection rate of micrometastases via ultrastaging emphasizes the importance of comprehensive pathological assessment.
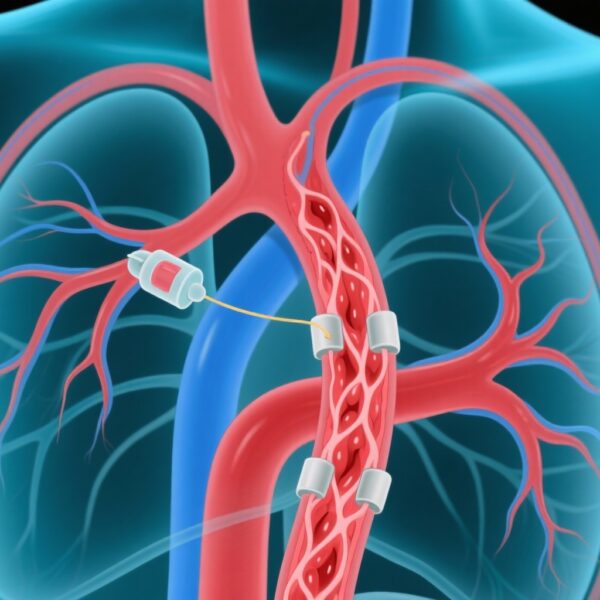
Implementing SLN biopsy could significantly reduce surgical morbidity and improve quality of life without compromising oncologic control, aligning with recent guideline trends favoring less invasive staging procedures. However, longer follow-up and validation in larger, diverse populations are necessary before universal adoption.
Limitations include the non-randomized design and potential variability in ultrastaging techniques across centers. Future studies should also evaluate the cost-effectiveness and impact on fertility preservation.
Conclusion and Future Directions
The SENTIX trial marks a pivotal shift toward precision surgical management in early-stage cervical cancer. It demonstrates that sentinel lymph node biopsy, combined with ultrastaging, can reliably guide treatment while minimizing surgical morbidity.
These findings could influence updates in clinical guidelines, promoting a less invasive approach that maintains oncologic safety. Continued research should focus on long-term outcomes, refinement of ultrastaging protocols, and integration into fertility-preserving strategies where appropriate.