Background
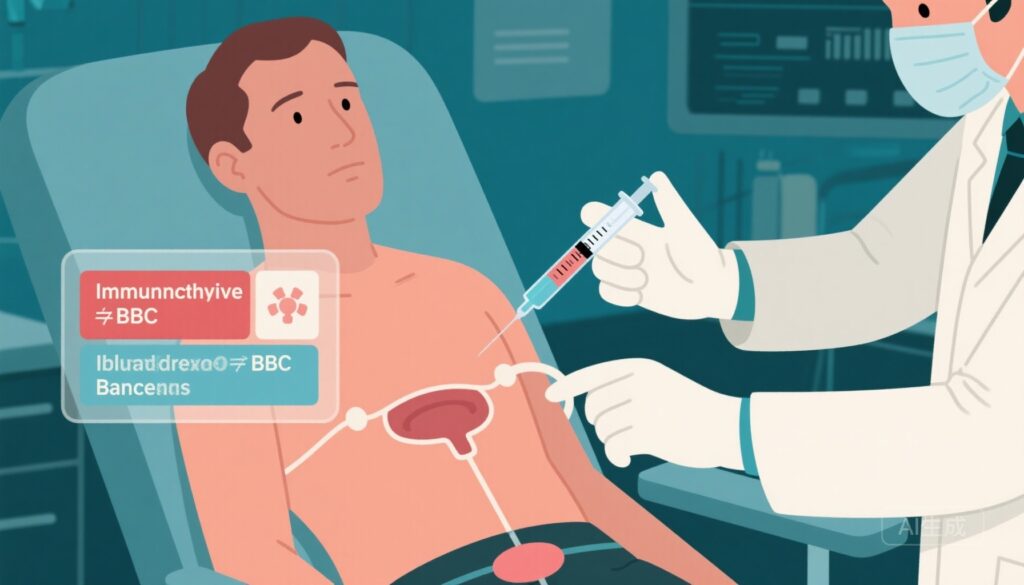
Non-muscle-invasive bladder cancer (NMIBC) is a type of bladder cancer that has not spread into the muscle layer of the bladder wall. High-risk NMIBC patients are particularly vulnerable to disease recurrence and progression even after treatment with transurethral resection of bladder tumor (TURBT) followed by Bacillus Calmette-Guérin (BCG) therapy, which is currently the standard intravesical immunotherapy aimed at preventing recurrence.
Despite BCG’s efficacy, many patients experience relapse or disease progression over time. This has spurred research into novel combination therapies to improve long-term outcomes. Durvalumab, a programmed death-ligand 1 (PD-L1) inhibitor, is an immune checkpoint inhibitor that helps enhance the body’s immune response against cancer cells. Combining durvalumab with BCG therapy might have additive or synergistic effects that could better control tumor recurrence and progression in this high-risk group.
Objectives
The primary goal of the POTOMAC (Durvalumab in Combination with BCG for BCG-Naive, High-Risk NMIBC) phase 3 trial was to determine whether adding systemic durvalumab to BCG induction and maintenance therapy improves disease-free survival compared to BCG therapy alone in patients newly diagnosed with high-risk NMIBC who had not previously received BCG treatment.
Study Design and Methods
This was a randomized, open-label, phase 3 clinical trial enrolling patients aged 18 years or older with BCG-naive, high-risk NMIBC who had undergone TURBT. High-risk NMIBC included patients with carcinoma in situ or high-grade tumors, known to have higher risk for recurrence and progression.
Participants were assigned in a 1:1:1 ratio to the following groups:
- Durvalumab plus BCG induction and maintenance: Patients received intravenous durvalumab every 4 weeks for 13 cycles, alongside intravesical BCG induction therapy given weekly for 6 weeks, followed by maintenance BCG doses at weeks 12, 24, 48, 72, and 96 (three weekly doses at each maintenance interval).
- Durvalumab plus BCG induction only: Patients received durvalumab with BCG induction but did not receive maintenance BCG.
- Comparison group (BCG induction and maintenance only): Patients received BCG induction and maintenance therapy alone.
The primary endpoint was investigator-assessed disease-free survival—defined as the time from randomization until the first recurrence of bladder tumor or death from any cause—in the durvalumab plus BCG induction and maintenance group versus the comparison group, analyzed in the intention-to-treat population.
The trial was registered on ClinicalTrials.gov (NCT03528694) and EudraCT (2017-002979-26) and was ongoing at the time of analysis, though no longer enrolling new participants.
Results
Between June 2018 and October 2020, 1,350 patients were screened, and 1,018 eligible patients were randomized:
- Durvalumab plus BCG induction and maintenance group: 339 patients (99% initiated treatment; 53% completed planned treatment)
- Durvalumab plus BCG induction only group: 339 patients (99% initiated; 71% completed)
- Comparison group (BCG induction and maintenance alone): 340 patients (over 99% initiated; 54% completed)
Median follow-up was approximately 60.7 months (range 51.5–66.5 months). The durvalumab plus BCG induction and maintenance group had 67 disease-free survival events (20%), while the comparison group had 98 events (29%). This translated to a statistically significant 32% relative reduction in risk of recurrence or death with the combination versus BCG alone (hazard ratio [HR] 0.68; 95% confidence interval [CI], 0.50–0.93; log-rank p=0.015).
Safety analyses showed grade 3 or 4 treatment-related adverse events occurred in 21% of patients in the durvalumab plus BCG induction and maintenance group, 15% in the durvalumab plus BCG induction only group, and 4% in the BCG-only group. Importantly, there were no treatment-related deaths. The adverse event profile was consistent with both therapies’ known safety profiles, and the combination’s side effects were manageable.
Interpretation and Clinical Implications
This study provides strong evidence that adding durvalumab immunotherapy to the current standard of care BCG induction and maintenance therapy meaningfully improves disease-free survival in patients with high-risk, BCG-naive NMIBC. This improvement is clinically important because it potentially reduces the risk of tumor recurrence and progression, which are frequent challenges in this patient population.
Furthermore, the combination did not result in unexpected or unacceptable toxicity, supporting its feasibility and safety in routine clinical use.
Overall, these results advocate for considering durvalumab combined with BCG induction and maintenance as a new treatment standard for high-risk NMIBC patients who have not received BCG previously. Optimizing and personalizing therapy for this group is critical to improving long-term outcomes and reducing the burden of bladder cancer recurrence and progression.
Future Directions
Further research could investigate biomarkers predicting response to immunotherapy combinations, explore durability of responses over longer follow-up, and assess quality of life outcomes compared to BCG alone. Additionally, studies might explore sequencing or combining durvalumab with other emerging treatments for NMIBC.
Funding and Acknowledgments
The trial was funded by AstraZeneca. The authors declare this study as the product of a large international consortium of investigators dedicated to improving bladder cancer therapy.
Reference
De Santis M, Palou Redorta J, Nishiyama H, et al. Durvalumab in combination with BCG for BCG-naive, high-risk, non-muscle-invasive bladder cancer (POTOMAC): final analysis of a randomised, open-label, phase 3 trial. Lancet. 2025 Nov 8;406(10516):2221-2234. doi:10.1016/S0140-6736(25)01897-5.