Highlight
- The CHINOREC trial evaluated the combination of dual immune checkpoint inhibitors (ipilimumab and nivolumab) with neoadjuvant chemoradiotherapy in rectal cancer.
- This regimen was found to be safe and feasible without increasing surgical complications or reoperation rates.
- Complete pathological response rates were similarly high in both groups but showed no statistically significant improvement with the addition of dual checkpoint blockade.
- The study supports further translational research to optimize integration and patient selection for combined immunoradiotherapy.
Study Background and Disease Burden
Rectal cancer remains a global health challenge, with significant morbidity and mortality despite advances in multimodal treatment. Standard care for locally advanced rectal cancer involves neoadjuvant chemoradiotherapy (CRT) followed by surgical resection. While immune checkpoint inhibitors (ICIs) have revolutionized treatment paradigms in multiple solid tumors, their efficacy in microsatellite-stable (MSS) rectal cancer has been limited due to tumor immune evasion and low immunogenicity.
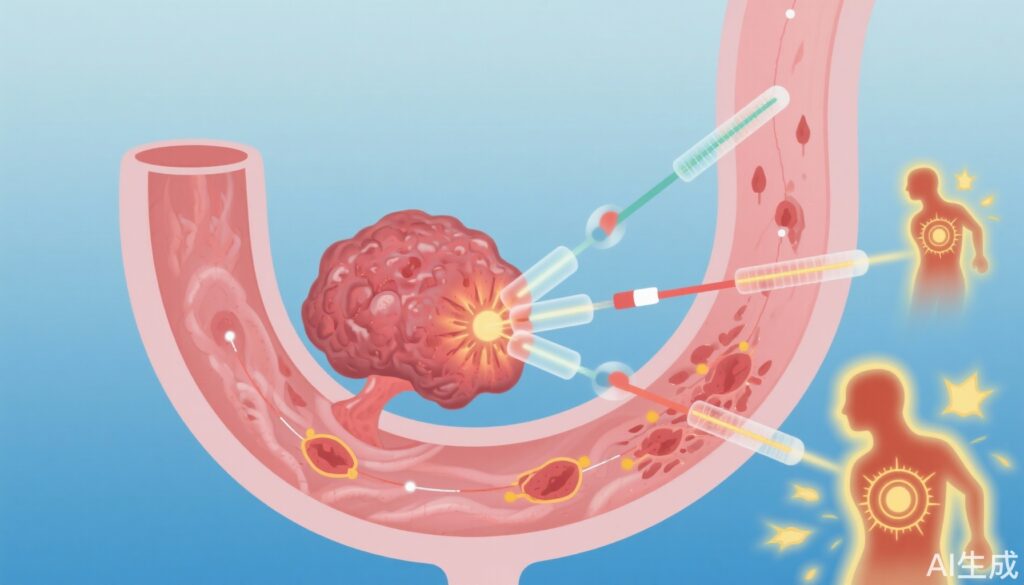
Recent evidence suggests that radiotherapy can modulate the tumor microenvironment to enhance immune recognition by increasing tumor antigen exposure and promoting T-cell infiltration. This has prompted investigation into combining ICIs with CRT to overcome resistance in MSS rectal cancer. Notably, anti-programmed cell death protein 1 (PD-1) monotherapy as part of neoadjuvant regimens has yielded encouraging complete response rates; however, the additional value of targeting cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) alongside PD-1 remains unclear.
Study Design
The CHINOREC trial was a prospective, randomized, open-label, multicenter phase 2 clinical study conducted at academic and tertiary centers in Austria from June 2, 2020, to March 15, 2024. The trial enrolled patients with locally advanced rectal cancer who were randomized in a 1:2 ratio to receive either standard neoadjuvant CRT alone or CRT combined with dual ICIs (ipilimumab plus nivolumab).
The neoadjuvant CRT protocol comprised radiotherapy delivering 50 Gy in 25 fractions (2 Gy each) along with concurrent capecitabine at 1650 mg/m2 daily. The experimental arm additionally received intravenous ipilimumab (1 mg/kg on day 7) and nivolumab (3 mg/kg every two weeks starting on day 14). Surgical resection was scheduled 10 to 12 weeks after completion of CRT. The primary endpoint was assessing safety and feasibility, specifically examining surgical complication rates and reoperations. Secondary endpoints included clinical and pathological response rates.
Key Findings
Out of 145 screened patients, 80 were randomized: 30 to CRT alone and 50 to CRT plus ipilimumab and nivolumab. The median age was 60 years, with 61% male participants.
Surgical complication rates were comparable between groups (77% in both arms) with no significant difference in reoperation rates (8% vs 7%, P > .99). Importantly, integrating dual immune checkpoint blockade did not increase surgical morbidity.
Regarding efficacy, major pathological response rates were similarly high (38% CRT vs 37% CRT-plus-ICI, P > .99), as were complete response rates (30% CRT vs 22% CRT-plus-ICI, P = .44), without statistically significant differences. These data reveal that while the dual ICI regimen shows clinical activity, it did not confer a clear advantage over CRT alone in this trial setting.
Expert Commentary
This trial provides important clinical evidence reinforcing the safety of combining dual ICIs with neoadjuvant CRT in rectal cancer. The lack of significant improvement in complete response rates underscores the biologic complexity of MSS rectal tumors and the challenge in overcoming their innate resistance to immunotherapy.
Potential factors influencing outcomes include the timing and sequencing of immunotherapy, ICI dosing, and radiation fractionation, all of which warrant further exploration. Future studies might investigate biomarkers predictive of response to better select patients who may benefit from combined immunoradiotherapy.
Additionally, mechanistic insights into how CTLA-4 blockade may synergize with PD-1 inhibition after radiotherapy in rectal cancer remain limited. Translational research integrating tumor genomics, immune profiling, and radiobiology will help optimize therapeutic strategies.
Conclusion
The CHINOREC trial establishes that adding ipilimumab and nivolumab to standard neoadjuvant CRT in rectal cancer is feasible and safe, without increasing surgical risks. Although this dual immune checkpoint inhibition approach did not significantly improve complete response rates compared to CRT alone, it demonstrated promising clinical activity that justifies further investigation.
These findings emphasize the need for continued translational and clinical research to refine the integration of immunotherapy with radiation, optimize patient selection, and ultimately improve outcomes for patients with locally advanced rectal cancer.
References
Laengle J, Kuehrer I, Kulu A, Kabiljo J, Ammon D, Zirnbauer R, et al. Dual Immune Checkpoint Inhibition Plus Neoadjuvant Chemoradiotherapy in Rectal Cancer: A Randomized Clinical Trial. JAMA Netw Open. 2025 Aug 1;8(8):e2527769. doi: 10.1001/jamanetworkopen.2025.27769. PMID: 40844778.