Highlight
– Sonelokimab, a bivalent nanobody targeting IL-17A and IL-17F, met the primary endpoint (ACR50 at week 12) in active psoriatic arthritis (PsA) at both 60 mg and 120 mg doses with induction dosing.
– High rates of ACR20, PASI90 and composite high‑threshold outcomes (ACR70+PASI100, minimal disease activity) were observed through 24 weeks in sonelokimab-treated patients.
– Safety was consistent with the IL-17 inhibition class: predominantly mild-to-moderate infections and a small number of oral candidiasis cases; no new safety signals reported over 24 weeks.
Background: disease burden and therapeutic rationale
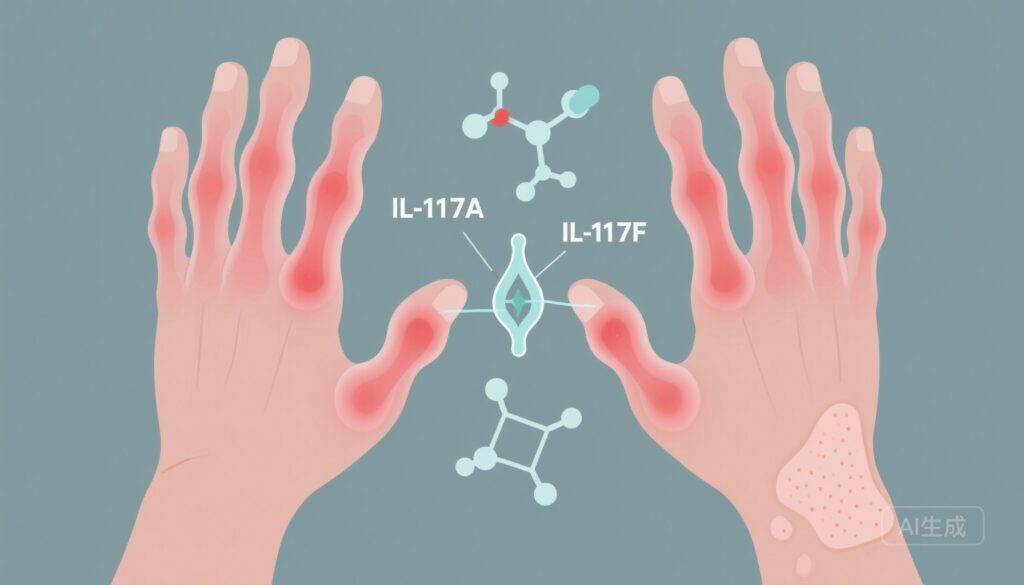
Psoriatic arthritis (PsA) is a heterogeneous, immune-mediated inflammatory disease that commonly combines peripheral arthritis, enthesitis, dactylitis, axial disease and psoriasis. It carries a significant burden of pain, disability and quality-of-life impairment and may lead to joint damage and reduced work capacity. Interleukin‑17 (IL‑17) family cytokines — especially IL‑17A and IL‑17F — play central roles in psoriatic skin and joint inflammation by promoting neutrophil recruitment, keratinocyte activation and synovial inflammation. Existing biologic therapies directed against IL‑17A (for example, secukinumab, ixekizumab) and dual IL‑17A/F inhibition (approaches under clinical development) have established the IL‑17 axis as a valid target in PsA.
Study design
The study reported by McInnes et al. was a randomized, double-blind, placebo-controlled phase 2 trial (ClinicalTrials.gov NCT05640245) that enrolled adults with active PsA. Overall, 207 patients were randomized to receive sonelokimab (SLK) at three different schedules — SLK 120 mg every 4 weeks (Q4W) with induction dosing (WI), SLK 60 mg Q4W with induction, or SLK 60 mg Q4W without induction — as well as a placebo (PBO) group and an adalimumab reference arm. The induction regimen (WI) provided an initial intensified exposure intended to achieve early disease control. The primary efficacy endpoint was the proportion of patients achieving an American College of Rheumatology 50% improvement (ACR50) at week 12. Key secondary endpoints included ACR20, PASI90 for concomitant skin disease, and minimal disease activity (MDA). Exploratory endpoints included composite high‑threshold outcomes such as ACR70 + PASI100 at week 24.
Key findings
Primary endpoint (ACR50 at week 12)
Both sonelokimab doses with induction met the primary outcome. ACR50 responses at week 12 were 46.3% (19/41) for the 60‑mg WI group (odds ratio [OR] vs placebo = 3.6; 95% confidence interval [CI] 1.3–9.9; P < 0.05) and 46.5% (20/43) for the 120‑mg WI group (OR = 4.0; 95% CI 1.4–11.3; P < 0.01). By comparison, placebo achieved an ACR50 of 20.0% (8/40).
Secondary joint and skin outcomes
Sonelokimab produced large and statistically significant improvements in other efficacy measures at week 12. ACR20 rates were 78.0% (32/41) for 60‑mg WI (P < 0.001) and 72.1% (31/43) for 120‑mg WI (P = 0.002), compared with 37.5% (15/40) for placebo. For patients with qualifying psoriasis at baseline, PASI90 at week 12 was achieved by 76.9% (20/26) in the 60‑mg WI group (P < 0.001) and 59.3% (16/27) in the 120‑mg WI group (P = 0.003), versus 15.4% (4/26) with placebo. These skin responses are notable for their magnitude and rapidity relative to expectations from IL‑17 pathway blockade.
Durability and high‑threshold composite responses at week 24
By week 24, sonelokimab-treated patients demonstrated robust and durable responses on higher‑bar outcomes. An exploratory composite endpoint of ACR70 + PASI100 was achieved by up to 48% (13/27) in the 120‑mg WI group. Minimal disease activity — a multidomain target reflecting joint and skin control and patient-reported elements — was reached in as many as 61% (25/41) of patients in the 60‑mg WI group. These high‑threshold responses suggest substantial multi‑domain disease control in a meaningful proportion of patients.
Comparative arm
The trial included adalimumab as a reference arm; however, the primary report focuses on comparisons versus placebo and does not present a formal, adequately powered head‑to‑head efficacy comparison between sonelokimab and adalimumab. Therefore, while the adalimumab arm provides context for expected responses with a TNF inhibitor, the study was not designed or powered to establish superiority or non‑inferiority versus adalimumab.
Safety and tolerability
Sonelokimab was generally well tolerated over the reporting period. The most common treatment‑emergent adverse events (TEAEs) were nasopharyngitis (60 mg = 6.1%; 120 mg = 5.2%), upper respiratory tract infection (60 mg = 6.1%; 120 mg = 4.1%), injection‑site erythema (60 mg = 3.7%; 120 mg = 3.1%) and headache (60 mg = 2.4%; 120 mg = 4.1%). Four instances of oral candidiasis were reported (60 mg = 2.4%; 120 mg = 2.1%), all described as mild to moderate, which aligns with the known predisposition to mucocutaneous candidiasis observed with IL‑17 pathway inhibition. No unexpected or severe safety signals were highlighted in the trial synopsis; longer follow‑up and larger cohorts will be required to better define rarer adverse events and long‑term safety.
Interpretation and expert commentary
The data demonstrate that dual IL‑17A/IL‑17F blockade with sonelokimab can achieve rapid, clinically meaningful improvements in both joint and skin domains in PsA, including high rates of skin clearance and substantial proportions achieving stringent composite outcomes. The magnitude of PASI90 and composite ACR70 + PASI100 responses is particularly encouraging for patients with high skin and joint disease burden.
Mechanistically, targeting both IL‑17A and IL‑17F aims to neutralize overlapping and potentially synergistic proinflammatory signals in psoriatic disease; sonelokimab — a nanobody platform with high affinity for both cytokines and inhibition of homodimeric and heterodimeric forms — exemplifies a biologic design intended to maximize blockade of the IL‑17 axis. Clinically, this approach may confer greater efficacy in skin clearance and possibly in certain joint manifestations, though definitive comparative data against IL‑17A‑only agents or other classes (TNF inhibitors, IL‑23 inhibitors, JAK inhibitors) are needed.
From a safety standpoint, the observed events mirror class effects (predisposition to mucocutaneous candidiasis and increased upper respiratory infections). Vigilance for fungal infections and other IL‑17–related safety issues will be important in later‑phase trials and real‑world use.
Limitations and considerations
Key limitations should temper interpretation: this is a phase 2 trial with modest sample sizes per arm and a relatively short controlled follow‑up (24 weeks reported). The trial included an adalimumab reference arm but was not powered for definitive head‑to‑head comparisons, limiting direct efficacy and safety comparisons with established biologic therapies. Details on prior biologic exposure, baseline disease subphenotypes (for example, axial involvement), or concomitant DMARD use were not extensively discussed in the summary; these factors influence both efficacy and generalizability. Finally, longer-term efficacy durability, radiographic progression outcomes and safety in larger, more diverse populations remain to be established in phase 3 programs.
Clinical implications and research directions
If phase 3 trials confirm these findings, sonelokimab could offer a potent multi‑domain therapeutic option for PsA, particularly in patients with substantial skin disease and those requiring high‑threshold responses. Areas for future research include: pragmatic head‑to‑head comparisons with IL‑17A inhibitors, TNF inhibitors and IL‑23 inhibitors; assessment in patients with predominant axial disease; long‑term safety and infection risk profiling; effects on radiographic progression; and identification of biomarkers that predict response or risk of adverse events. Health‑economic analyses will also be needed to place sonelokimab within existing treatment algorithms and reimbursement frameworks.
Conclusion
Sonelokimab demonstrated significant and clinically meaningful improvements in joint and skin outcomes in active PsA compared with placebo in this phase 2 randomized trial. The magnitude of responses, including high PASI90 rates and meaningful proportions achieving composite high‑threshold endpoints, supports further clinical development. Safety signals were consistent with IL‑17 pathway inhibition. Phase 3 studies are warranted to confirm efficacy, define long‑term safety, and position sonelokimab relative to available biologic therapies.
Funding and trial registration
ClinicalTrials.gov: NCT05640245. Full trial funding and disclosures are reported in the primary publication (McInnes IB et al., Nature Medicine, 2025).
Reference
McInnes IB, Coates LC, Mease PJ, Ogdie A, Kavanaugh A, Eder L, Schett G, Kivitz A, McGonagle D, Brennan N, Godwood A, Cullen E, Reich K, Ritchlin CT, Merola JF. Sonelokimab, an IL-17A/IL-17F-inhibiting nanobody for active psoriatic arthritis: a randomized, placebo-controlled phase 2 trial. Nat Med. 2025 Oct 6. doi: 10.1038/s41591-025-03971-6. Epub ahead of print. PMID: 41053449.