Highlights
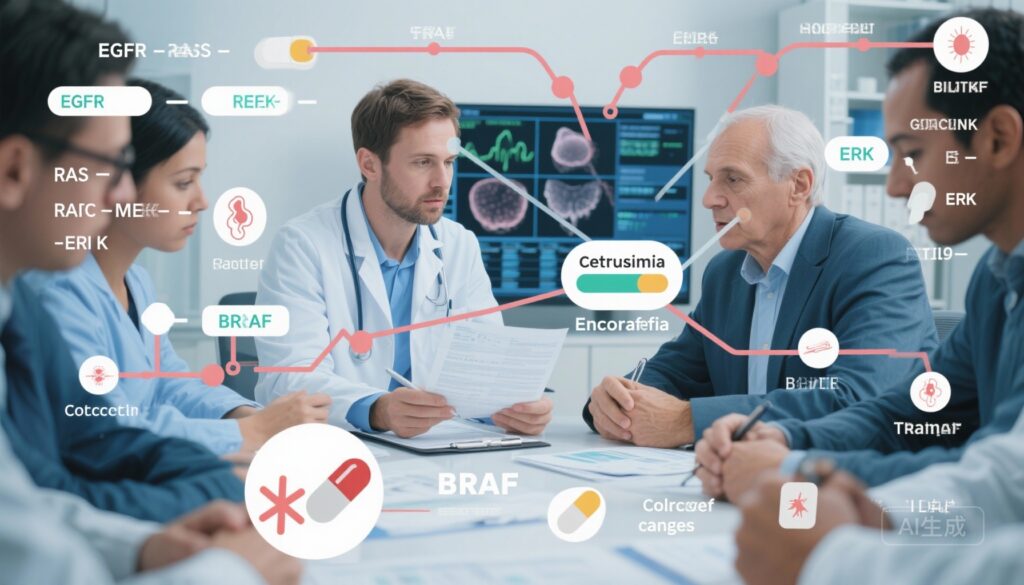
– Network meta‑analysis of 60 studies with 4,633 patients supports anti‑EGFR/BRAF combinations as the therapeutic backbone for advanced BRAF‑mutated colorectal cancer (mCRC).
– In first‑line treatment, doublet chemotherapy plus anti‑EGFR/BRAF (the “doublet‑double‑target” approach) produced the largest overall survival benefit (HR vs DCT‑anti‑VEGF 0.49, 95% CrI 0.36–0.66).
– In second or later lines, anti‑EGFR/BRAF regimens, with or without MEK inhibition, ranked highest for efficacy and tolerability.
Background and clinical context
BRAF‑mutations (most commonly V600E) occur in approximately 5–10% of colorectal cancers and define a clinicopathologic subset with aggressive behaviour, frequent right‑sided tumours, poor prognosis, and limited responsiveness to standard cytotoxic regimens. Historically, guideline recommendations for fit patients prioritized intensive chemotherapy such as a triplet (FOLFOXIRI) plus anti‑VEGF (bevacizumab) to try to maximise cytoreduction. However, targeted inhibition of the driver BRAF mutation (and its adaptive feedback via EGFR) has emerged as a rational strategy. The optimal way to combine cytotoxic chemotherapy and targeted agents, and the best targeted partner(s) (EGFR, MEK, PI3K) across treatment lines, has remained uncertain.
Study design
The paper by Professor Zang Yuansheng and colleagues from the Department of Oncology, The Second Affiliated Hospital of Naval Medical University (Shanghai Changzheng Hospital) reports a systematic review and network meta‑analysis (PROSPERO CRD420250653959) that searched PubMed, Embase, Cochrane Library and ClinicalTrials.gov up to 31 May 2025, plus conference proceedings. Sixty clinical trials and multicentre real‑world studies were included, covering 4,633 patients with advanced BRAF‑mutated colorectal cancer.
Primary endpoint: overall survival (OS) in first‑line and second/later‑line settings. Secondary endpoints: progression‑free survival (PFS), objective response rate (ORR), disease control rate (DCR), and grade ≥3 adverse events (AEs).
Analytical approach: single‑arm meta‑analysis, pairwise meta‑analysis, and Bayesian network meta‑analysis (NMA) were performed. Outcomes were pooled as hazard ratios (HRs) with 95% credible intervals (CrIs) for time‑to‑event endpoints and odds ratios for dichotomous outcomes. Rankograms and SUCRA (surface under the cumulative ranking curve) scores evaluated relative regimen performance.
Key findings
Overall evidence base: 60 studies, 4,633 patients; data synthesis integrated randomized trials, single‑arm trials and observational cohorts to compare modern targeted strategies and chemotherapy backbones across lines of therapy.
First‑line therapy
Main result: combining doublet chemotherapy with anti‑EGFR/BRAF therapy delivered the best OS among first‑line targeted strategies. Notable comparisons (first‑line):
- DCT (doublet chemotherapy: typically two cytotoxic agents) + anti‑EGFR/BRAF vs DCT + anti‑VEGF: HR for OS 0.49 (95% CrI 0.36–0.66).
- DCT + anti‑EGFR/BRAF vs triplet chemotherapy + anti‑VEGF: HR 0.51 (95% CrI 0.33–0.80).
- DCT + anti‑EGFR/BRAF vs anti‑EGFR/BRAF alone (no chemo): HR 0.70 (95% CrI 0.51–0.96).
SUCRA rankings for first‑line strategies placed DCT‑anti‑EGFR/BRAF highest for OS (SUCRA 0.94) and PFS (0.93), with SCT (single agent chemotherapy)‑anti‑EGFR/BRAF also performing strongly (OS SUCRA 0.90, PFS 0.92). These findings indicate that adding a targeted EGFR/BRAF double blockade to a modest chemotherapy backbone provides a larger survival advantage than either chemotherapy intensification with anti‑VEGF or targeted therapy alone.
Second‑line and later therapy
In previously treated patients, targeting EGFR/BRAF remained the most effective approach. Regimens combining anti‑EGFR and BRAF inhibitors, with or without a MEK inhibitor (e.g., the BEACON strategy), ranked highest across endpoints (OS, PFS, ORR) and generally showed acceptable tolerability compared with alternative strategies. The NMA supports the established role of encorafenib + cetuximab (± binimetinib) and similar combinations in later lines where prior cytotoxic therapy has been delivered.
Objective response and disease control
Anti‑EGFR/BRAF combinations (with chemotherapy in first line, and with or without MEK inhibitors later) produced higher ORRs and DCRs than comparator regimens in pooled analyses; the magnitude of benefit was clinically meaningful, especially when chemotherapy was included in the first line.
Safety and tolerability
Grade ≥3 adverse events were reported across regimens. The NMA found that anti‑EGFR/BRAF regimens, particularly when used without intensive chemotherapy, had manageable toxicity profiles. The first‑line DCT‑anti‑EGFR/BRAF approach increased treatment intensity compared with single‑agent targeted therapy but retained a tolerability profile that the authors deemed acceptable for appropriately selected, fit patients. As with all intensified combinations, clinician judgment regarding fitness, comorbidity and patient preferences remains essential.
Interpretation and mechanistic plausibility
The NMA converges on a biologically plausible conclusion: BRAF‑mutant colorectal cancers are driven by aberrant MAPK signalling, but single‑agent BRAF inhibition triggers rapid adaptive feedback via EGFR activation in colorectal cancer (unlike melanoma). Concurrent EGFR blockade restores and prolongs pathway suppression, and adding cytotoxic chemotherapy in the first line plausibly improves initial tumour control by both cytoreductive and signalling‑directed mechanisms. The data therefore support a “dual‑target plus cytotoxic” paradigm early, with targeted doublets preserved as highly active salvage options.
Clinical implications
For fit patients with newly diagnosed advanced BRAF‑mutated mCRC, the evidence supports combining doublet chemotherapy with anti‑EGFR/BRAF therapy as the preferred first‑line strategy to maximise overall survival. For patients who have already received prior systemic therapy, anti‑EGFR/BRAF regimens (for example, encorafenib + cetuximab ± binimetinib per BEACON‑type approaches) remain the most effective and tolerable options.
The authors from Shanghai Changzheng Hospital (臧远胜, Qin Baodong as first author, and other co‑authors) highlight an institutional regimen termed the “IMPROVEMENT” or “double‑target double‑chemo” (双靶双化) “Long March” scheme, previously reported in a single‑centre phase II study with high ORR (reported in European Journal of Cancer, 2022). The current NMA integrates that body of evidence and positions the approach within the comparative landscape, offering higher‑level support for a stratified strategy: intensified, double‑targeted cytotoxic therapy in first line, and targeted‑only doublets in later lines to preserve efficacy while improving tolerability.
Limitations and areas for caution
Despite the large pooled sample, several important limitations should be noted:
- Heterogeneity in included studies: the NMA pooled randomized trials, single‑arm phase II series and real‑world cohorts with differing inclusion criteria, regimens, dosing, and outcome ascertainment.
- Potential for selection bias: many intensification strategies were tested in selected, fitter populations, which may amplify apparent benefit versus more heterogeneous real‑world patients.
- Limited head‑to‑head randomized data comparing the exact combinations in question (for example, prospective randomized comparisons of DCT‑anti‑EGFR/BRAF vs triplet chemo + bevacizumab are lacking), so inferences rely on indirect comparisons in the network.
- Aggregate data meta‑analysis cannot fully account for patient‑level prognostic factors (e.g., microsatellite status, performance status, metastatic burden), which are important effect modifiers.
Expert commentary and guideline context
These findings align with the mechanistic rationale and the positive randomized evidence supporting anti‑EGFR/BRAF combinations in later lines (BEACON). They also challenge the reflexive use of triplet chemotherapy + bevacizumab as the universal first‑line approach for all BRAF‑mutant patients, suggesting instead a nuanced, stratified plan: intensified, targeted cytotoxic therapy for fit patients at diagnosis (to achieve maximal early control), with targeted doublets reserved as potent and better‑tolerated later options.
Implementation should consider patient fitness, organ function, symptoms, and rapidity of disease progression. Where rapid cytoreduction is required, an intensified regimen that includes chemotherapy may still be needed. Molecular profiling (confirming BRAF V600E and testing for MSI status, RAS mutations, HER2 and upstream alterations) remains mandatory to guide therapy and clinical trial selection.
Conclusions and next steps
The BMJ systematic review and network meta‑analysis represents the largest synthesis to date for advanced BRAF‑mutated colorectal cancer. It supports a treatment paradigm in which anti‑EGFR/BRAF double targeting is the therapeutic backbone; adding doublet chemotherapy in the first line confers the largest survival benefit. In later lines, anti‑EGFR/BRAF regimens (with or without MEK inhibitors) offer the best balance of efficacy and tolerability.
Future work should prioritise randomized comparisons of chemotherapy backbones combined with targeted doublets, deeper molecular stratification to personalise the intensity of therapy, and prospective real‑world studies to confirm tolerability and generalizability across broader patient populations.
Funding and trial registration
The systematic review was prospectively registered at PROSPERO CRD420250653959. The BMJ article citation: Targeted therapy in advanced BRAF‑mutated colorectal cancer: systematic review and network meta‑analysis. BMJ 2025;391 doi: https://doi.org/10.1136/bmj-2025-086026 (Published 19 November 2025).
Selected references
– Kopetz S, et al. Encorafenib, binimetinib, and cetuximab in BRAF V600E‑mutated colorectal cancer. N Engl J Med. 2019;381:1632–1643.
– Targeted therapy in advanced BRAF‑mutated colorectal cancer: systematic review and network meta‑analysis. BMJ 2025;391:e086026. doi:10.1136/bmj-2025-086026.
– Institutional phase II report of the “IMPROVEMENT” double‑target double‑chemo (臧远胜 team). European Journal of Cancer, 2022 (reported by Shanghai Changzheng Hospital team).
Correspondence and media events: On 20 November, Shanghai Changzheng Hospital held a press briefing to present these clinical research results online. The study’s corresponding author is Professor 臧远胜; Qin Baodong is the first author; co‑first authors include 焦晓栋, 王湛, and 柳珂, all from the Department of Oncology, The Second Affiliated Hospital of Naval Medical University (Shanghai Changzheng Hospital).