ST-segment elevation myocardial infarction (STEMI) remains a critical cardiovascular emergency demanding timely revascularization to restore coronary blood flow and minimize myocardial damage. Primary percutaneous coronary intervention (PCI) with immediate stent implantation is the guideline-recommended standard of care. However, immediate stenting can sometimes exacerbate microvascular injury through distal embolization of thrombotic material, microvascular obstruction, and impaired coronary flow, collectively heightening adverse cardiac outcomes such as heart failure and death. These complications underscore the clinical interest in exploring deferred stent implantation, whereby stenting is postponed after initial reperfusion to allow stabilization and thrombus burden reduction. The DANAMI-3-DEFER trial was designed to investigate the long-term clinical impact of deferred compared to conventional immediate stenting in STEMI patients.
Study Design
The DANAMI-3-DEFER (Third Danish Study of Optimal Acute Treatment of Patients With STEMI – Deferred Stent Implantation Versus Conventional Treatment) was a multicenter, open-label, randomized controlled trial conducted at four PCI centers in Denmark. Eligible patients were adults presenting within 12 hours of symptom onset with STEMI, defined by standard electrocardiographic criteria.
Participants (N=1215) were randomized 1:1 to either deferred stent implantation (n=603), delayed more than 24 hours post initial reperfusion, or conventional immediate stenting (n=612). Patients in the deferred group required achievement of stable Thrombolysis in Myocardial Infarction (TIMI) flow grade II to III immediately after initial reperfusion. Post-procedure intravenous therapy with glycoprotein IIb/IIIa inhibitors or bivalirudin was recommended to minimize thrombotic complications.
The primary endpoint was a composite of hospitalization for heart failure or all-cause mortality, with key secondary endpoints including the individual components of the primary endpoint and target vessel revascularization. The study included extended follow-up for up to 10 years to assess long-term outcomes.
Key Findings
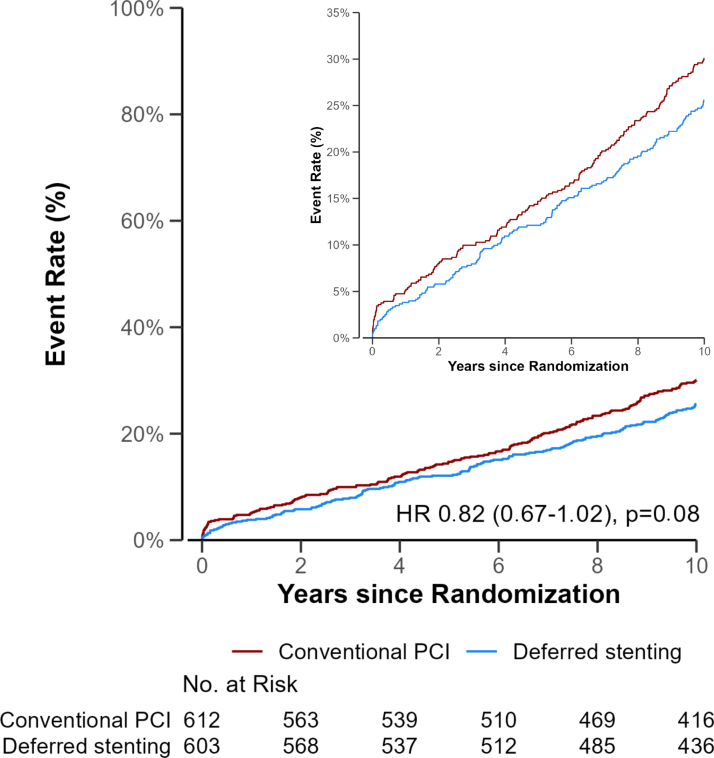
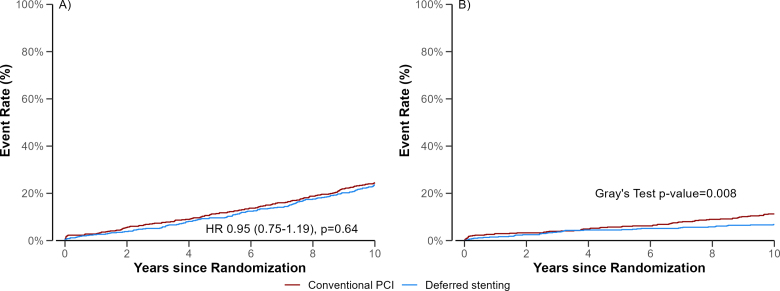
After a median follow-up of 10 years, the primary composite outcome occurred in approximately 35% of patients and was not statistically significantly reduced by deferred stenting compared to conventional PCI (hazard ratio [HR] 0.82, 95% confidence interval [CI] 0.67-1.02; P=0.08). Specifically, mortality rates were 24% vs. 25% (HR 0.95, 95% CI 0.75-1.19) in deferred and conventional groups, respectively, indicating no mortality difference.
Cumulative incidence of all-cause mortality or hospitalization for heart failure.
Cumulative incidence of all-cause mortality and hospitalization for heart failure.
Importantly, deferred stenting was associated with a significant reduction in hospitalizations for heart failure (odds ratio [OR] 0.58, 95% CI 0.39-0.88), suggesting a protective effect on cardiac function. Rates of target vessel revascularization did not differ significantly between groups (OR 1.20, 95% CI 0.81-1.79).
A substudy involving 1205 patients evaluated the angiographic outcomes and demonstrated that deferred stenting significantly lowered incidences of slow or no reflow (OR 0.60) and distal embolization (OR 0.67), particularly benefiting high-risk subgroups including patients older than 65 years, those with occluded culprit arteries, and patients with high thrombus burden (grade >3).
No significant differences in procedural complications such as myocardial infarction, bleeding, contrast-induced nephropathy, or stroke were observed, confirming comparable safety profiles.
Expert Commentary
The DANAMI-3-DEFER trial provides robust, decade-long evidence elucidating the nuanced role of deferred stenting in STEMI management. The lack of mortality benefit suggests that while deferred stenting may not improve survival, it confers a clear benefit in reducing heart failure hospitalizations, likely due to mitigated microvascular injury and distal embolization. These findings align with mechanistic insights that early thrombus stabilization and microvascular salvage contribute to preserved left ventricular function.
Despite the promising heart failure outcomes, deferred stenting did not reduce recurrent infarctions or need for repeat revascularization, indicating that the procedural timing may primarily influence myocardial remodeling rather than atherothrombotic progression.
Limitations include the open-label design and exclusion of certain high-risk subgroups, which may affect generalizability. Ongoing trials might further clarify patient selection criteria and refine this strategy.
Conclusion
In summary, the DANAMI-3-DEFER trial concludes that deferred stent implantation in STEMI patients does not significantly lower all-cause mortality or the composite of death and heart failure hospitalization at 10 years compared with conventional immediate stenting. However, deferred stenting favorably reduces hospitalizations for heart failure and angiographic markers of microvascular impairment such as slow/no reflow and distal embolization, especially in older patients and those with high thrombus burden.
These data suggest a tailored approach to immediate versus deferred stenting may optimize long-term cardiac function and patient outcomes. Clinicians should weigh the benefits of microvascular protection against the risks and logistical challenges of delaying stent implantation.
References
1. Marquard JM, Engstrøm T, Kelbæk H, et al. 10-Year Outcomes of Deferred or Conventional Stent Implantation in Patients With STEMI (DANAMI-3-DEFER). Circ Cardiovasc Interv. 2025;18(6):e015369. doi:10.1161/CIRCINTERVENTIONS.125.015369 IF: 7.4 Q1 .
2. Kelbæk H, Høfsten DE, Køber L, et al. Deferred versus conventional stent implantation in patients with ST-segment elevation myocardial infarction (DANAMI 3-DEFER): an open-label, randomised controlled trial. Lancet. 2016;387(10034):2199-2206. doi:10.1016/S0140-6736(16)30072-1 IF: 88.5 Q1 .
3. Nepper-Christensen L, Kelbæk H, Ahtarovski KA, et al. Angiographic outcome in patients treated with deferred stenting after ST-segment elevation myocardial infarction-results from DANAMI-3-DEFER. Eur Heart J Acute Cardiovasc Care. 2022;11(10):742-748. doi:10.1093/ehjacc/zuac098 IF: 4.6 Q1 .