Highlight
– Prospective cohort (N = 110) shows darker skin tone is associated with greater negative bias of forehead NIRS (INVOS 5100C) compared to mixed venous saturation.
– Mean bias in the darkest ITA categories was −12.8% versus −2.5% and +0.3% in lighter categories; skin tone (ITA) remained an independent predictor of bias.
– Findings raise concerns that single-device NIRS measurements may systematically misestimate cerebral oxygenation in children with darker skin, with potential implications for patient management and health equity.
Background
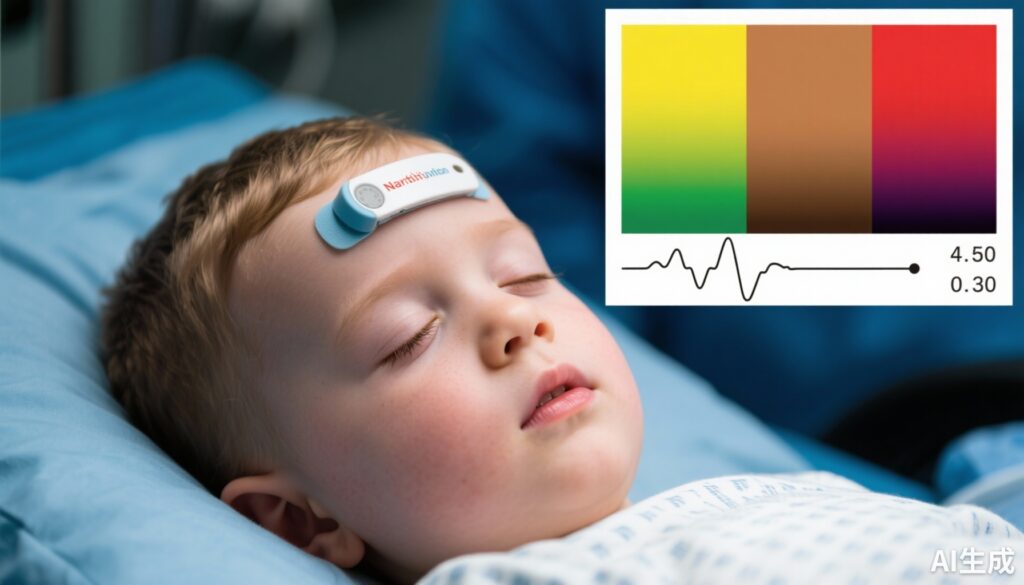
Near-infrared spectroscopy (NIRS) devices are widely used in perioperative and critical care to provide regional cerebral oxygen saturation (rSO2), informing clinicians about cerebral perfusion and oxygen delivery. Like pulse oximetry, NIRS is an optical technology that infers oxygenation from light absorption at multiple wavelengths. Recent high-profile work has demonstrated that pulse oximeters can show racial bias, overestimating arterial oxygen saturation in individuals who identify as Black or have darker skin pigmentation. Such measurement bias can influence clinical decisions and outcomes. Whether and how skin pigmentation influences NIRS performance has been less well quantified, particularly in children.
The study by Starnes et al. (Anesthesiology, 2025) prospectively investigated the association between objectively measured skin tone and performance of a commonly used cerebral NIRS device (INVOS 5100C) in children undergoing cardiac catheterization. The authors hypothesized that skin pigmentation would affect NIRS bias when compared with an invasive reference measure, mixed venous saturation (SvO2).
Study design
Population and setting
Consecutive patients under 21 years old undergoing cardiac catheterization at a single center were enrolled (N = 110). The cohort reflects children requiring invasive hemodynamic assessment and contains a range of congenital cardiac physiology; detailed comorbidity distribution is reported in the original manuscript.
Index test and reference standard
Regional oxygen saturation was recorded from a Medtronic INVOS 5100C NIRS sensor placed on the forehead. The reference comparator was mixed venous oxygen saturation (SvO2), obtained invasively during catheterization. Central venous measurements were used as a physiologic benchmark to assess how well the noninvasive NIRS reflected systemic venous oxygenation.
Skin tone measurement
Rather than using self-reported race or clinician-assigned categories, skin tone was quantified with spectrophotometry using the individual typology angle (ITA) — an objective metric based on reflectance that correlates with pigmentation. ITA values were categorized into ordered groups (lighter to darker) for comparison.
Analysis
Primary analysis compared the bias (NIRS − SvO2) across ITA categories. Multivariable linear regression assessed the independent association of ITA with NIRS bias, adjusting for relevant clinical covariates.
Key findings
Main result
The study found substantial differences in mean bias across skin tone groups. Patients in the darkest ITA categories (5 and 6) had a mean bias of −12.8% (NIRS lower than SvO2), compared with mean biases of −2.5% in ITA categories 3 and 4 and +0.3% in ITA categories 1 and 2. The differences were statistically significant: darker versus intermediate (difference 10.3%; 95% CI, 4.4 to 16.3; P < 0.001) and darker versus lightest (difference 13.1%; 95% CI, 7.5 to 18.7; P < 0.001).
In multivariable linear regression, ITA remained significantly associated with NIRS bias (coefficient 0.173; P < 0.001), indicating that increasing ITA (lighter skin) predicted less negative bias (or relatively higher NIRS values) after adjustment for measured covariates.
Interpretation of bias
A negative bias (NIRS reading lower than SvO2) in darker-skinned children implies the device reports lower regional oxygenation than the invasive venous reference. This pattern differs from the pulse oximetry problem highlighted in prior studies (where darker skin was linked to overestimation of arterial oxygen saturation). For cerebral NIRS, underestimation could prompt clinicians to escalate interventions (increase oxygen delivery, transfuse, alter hemodynamics) when they are not physiologically indicated, potentially exposing patients to unnecessary interventions. Conversely, if clinicians adjust thresholds based on suspected device bias, they may unwittingly undertreat patients who need intervention. Both scenarios raise safety and equity concerns.
Robustness and secondary findings
The association persisted in adjusted models, strengthening the case for a direct relation between skin pigmentation and NIRS signal interpretation for this device. The study used an objective skin-tone measurement (spectrophotometry) rather than race, reducing misclassification and making the finding about pigmentation biology rather than social constructs.
Mechanistic considerations
NIRS devices emit and detect near‑infrared light after some photons traverse tissue. The signal depends on absorption and scattering properties of skin, skull, and brain tissue. Melanin absorbs light across visible and parts of the near-infrared spectrum; higher melanin content can attenuate transmitted and reflected light, decreasing signal intensity or altering the relative absorption at the wavelengths used to distinguish oxy- and deoxyhemoglobin. Device algorithms assume certain optical pathlengths and baseline tissue composition; if melanin meaningfully changes the detected spectra, the oxygenation estimate can be biased. The study’s findings are biologically plausible given known optical properties of melanin and the analogous problems observed with pulse oximetry.
Clinical implications
– Monitoring and decision thresholds: Clinicians should be aware that a commonly used NIRS device may systematically report lower rSO2 in children with darker skin. Decisions that rely on fixed absolute NIRS thresholds (for example, to trigger interventions during cardiac surgery or postoperative monitoring) may need to account for possible device bias.
– Patient safety and equity: A device that performs differently across skin tones risks contributing to differences in care and outcomes if not identified and mitigated. Under- or over-treatment driven by measurement error can exacerbate disparities.
– Device selection and local validation: Institutions using NIRS for critical decision-making, particularly in diverse pediatric populations, should consider device-specific validation across the range of skin pigmentation represented among their patients.
Strengths and limitations
Strengths:
– Prospective design with consecutive sampling in a clinical setting.
– Objective, spectrophotometric measurement of skin tone (ITA) rather than race-based proxies.
– Use of an invasive physiologic reference (SvO2) for comparison.
Limitations:
– Single-device evaluation (Medtronic INVOS 5100C); results may not generalize to other manufacturers or newer-generation sensors.
– Single-center pediatric cohort undergoing cardiac catheterization — findings may not extend to adults, different patient populations, other probe sites (e.g., somatic NIRS), or non-cardiac settings.
– The reference, mixed venous saturation, is systemic and not a direct cerebral venous saturation; differences in physiology between central venous and cerebral venous beds could contribute to measurement discordance.
– The report provides group-level summary measures; individual patient variability and the distribution of values within ITA categories are important for clinical translation and were not fully described in the abstract.
Expert commentary and context
This study complements and extends concerns raised for pulse oximetry: optical monitoring devices can be susceptible to bias introduced by skin pigmentation. As with pulse oximeters, the problem is not necessarily the clinical intent but the incompleteness of device validation across biologic diversity. The use of spectrophotometric ITA is a methodological advance that should be adopted in future device testing and regulatory evaluations.
Manufacturers should prioritize multi-spectral device design, algorithmic re-calibration with diverse training data, and transparent reporting of performance stratified by objective pigmentation measures. Clinicians and guideline panels should weigh current evidence when recommending absolute rSO2 thresholds and incorporate awareness of potential device-related bias into practice.
Recommendations and next steps
– Replication: Multi-center studies that test multiple NIRS systems across broader age ranges, clinical contexts, and standardized timing relative to invasive samples are needed.
– Device-level evaluation: Manufacturers should publish performance stratified by objective skin-tone measures and, where needed, update algorithms or sensors to improve equity.
– Regulatory standards: Standards and validation guidelines should require enrollment of participants across a pre-specified distribution of objectively measured skin tones and report device accuracy and bias across these strata.
– Clinical guidance: Until broader validation exists, clinicians should interpret NIRS values in context, consider corroborating information (hemodynamics, lactate, invasive measures when available), and avoid lone reliance on absolute NIRS thresholds to make definitive treatment decisions in populations at risk for measurement bias.
Conclusion
Starnes et al. provide prospective evidence that darker skin pigmentation is associated with clinically meaningful negative bias in forehead NIRS readings using the INVOS 5100C in children. The study highlights a critical and actionable gap: optical monitoring tools must be validated across objective measures of skin pigmentation to ensure equitable performance. Addressing this will require collaboration among clinicians, researchers, device manufacturers, and regulators to update validation practices, improve device design, and protect patient safety across diverse populations.
Funding and clinicaltrials.gov
Funding: Not specified in the abstract provided. ClinicalTrials.gov: Not reported in the abstract provided.
References
1. Starnes JR, Welch W, Henderson C, Hudson S, McVean B, Risney S, Nicholson GT, Doyle TP, Janssen D, Londergan BP, Parra DA, Slaughter JC, Aliyu MH, Graves JA, Soslow JH. Near-infrared Spectroscopy and Skin Tone in Children: A Prospective Cohort Study. Anesthesiology. 2025 Nov 3:10.1097/ALN.0000000000005738. doi: 10.1097/ALN.0000000000005738. Epub ahead of print. PMID: 40880206; PMCID: PMC12520187.
2. Sjoding MW, Dickson RP, Iwashyna TJ, Gay SE, Valley TS. Racial bias in pulse oximetry measurement. N Engl J Med. 2020;383:2477–2478.
(Readers are encouraged to consult the full Starnes et al. manuscript for complete methods, subgroup analyses, and additional discussion.)

![[Lutetium-177]Lu-PSMA-617 Delays Quality-of-Life Decline, Pain Progression, and Symptomatic Skeletal Events in PSMA-Positive mCRPC: In-depth PSMAfore Analysis](https://news.medxy.ai/wp-content/uploads/2025/11/9d3c0201-d1b3-49f2-a408-3ea3d0347451-600x600.jpg)
