Highlight
– In patients with asymptomatic, high‑grade (≥70%) carotid stenosis, carotid‑artery stenting plus intensive medical management reduced the 4‑year incidence of a composite outcome (perioperative any stroke or death within 44 days, or subsequent ipsilateral ischemic stroke) compared with intensive medical management alone (6.0% vs 2.8%; P = 0.02).
– Carotid endarterectomy plus intensive medical management did not significantly reduce the 4‑year incidence of the same composite outcome compared with intensive medical management alone (5.3% vs 3.7%; P = 0.24).
– Early (day 0–44) procedural strokes and deaths were more common in the revascularization arms, underscoring a trade‑off between short‑term procedural risk and potential longer‑term prevention of ipsilateral stroke.
Background and Clinical Context
Asymptomatic carotid artery stenosis remains a common clinical dilemma. Historically, randomized trials (e.g., ACAS, ACST) demonstrated modest absolute stroke‑risk reductions with carotid endarterectomy relative to medical therapy, but those trials were conducted before modern risk‑factor management and widespread statin use. Over the past two decades, advances in antiplatelet therapy, statins, blood‑pressure control, smoking cessation, and diabetes care have substantially lowered baseline stroke risks, prompting reappraisal of routine revascularization for asymptomatic disease.
The CREST‑2 program was designed to test whether adding revascularization (either carotid‑artery stenting or carotid endarterectomy) to an intensive contemporary medical regimen affords additional protection against stroke among patients with high‑grade, asymptomatic carotid stenosis.
Study Design and Methods
CREST‑2 comprised two parallel, observer‑blinded randomized clinical trials conducted at 155 centers across five countries. Eligible patients had high‑grade (≥70%) asymptomatic carotid stenosis and were appropriate candidates for either stenting or endarterectomy; separate randomizations were used for the stenting and endarterectomy comparisons.
Participants were randomized to intensive medical management alone versus intensive medical management plus the assigned revascularization procedure (carotid‑artery stenting or carotid endarterectomy). Intensive medical management included aggressive risk‑factor control (antiplatelet therapy, high‑intensity statins, blood‑pressure targets, glycemic control where indicated, and lifestyle interventions). The primary composite outcome was any stroke or death from randomization to 44 days (perioperative window), or ipsilateral ischemic stroke occurring thereafter up to 4 years. Trials were observer‑blinded for outcome assessment.
Enrollment totaled 1,245 patients in the stenting trial and 1,240 patients in the endarterectomy trial.
Key Results
Primary outcome—stenting comparison
At 4 years, the incidence of the primary composite outcome in the stenting trial was 6.0% (95% CI, 3.8 to 8.3) in the medical‑therapy group and 2.8% (95% CI, 1.5 to 4.3) in the stenting group. The absolute difference favored stenting (absolute risk reduction ~3.2 percentage points) and was statistically significant (P = 0.02).
Early events (day 0 to 44) favored medical therapy: no strokes or deaths occurred in the medical‑therapy group during that window, while the stenting group experienced seven strokes and one death. Over the remainder of follow‑up (beyond day 44 to 4 years), the stenting group had fewer ipsilateral ischemic strokes than medical therapy, such that the cumulative 4‑year outcome favored stenting.
Interpretation: Although stenting incurred a measurable periprocedural risk, durable prevention of ipsilateral ischemic stroke during follow‑up produced a net benefit over 4 years in this trial population. The absolute 4‑year risk reduction of approximately 3.2% corresponds to a number needed to treat (NNT) of roughly 31 patients to prevent one primary outcome event over 4 years (this back‑of‑the‑envelope estimate should be interpreted cautiously and in the clinical context of perioperative risk and life expectancy).
Primary outcome—endarterectomy comparison
In the endarterectomy trial, the 4‑year incidence of the primary outcome was 5.3% (95% CI, 3.3 to 7.4) in the medical‑therapy group and 3.7% (95% CI, 2.1 to 5.5) in the endarterectomy group. The absolute difference was smaller than in the stenting comparison and did not reach statistical significance (P = 0.24).
Early events (day 0 to 44) included three strokes in the medical‑therapy group and nine strokes in the endarterectomy group. Over the remainder of follow‑up, endarterectomy did not yield a clear, statistically significant reduction in ipsilateral stroke compared with optimized medical care alone.
Safety and perioperative considerations
Both revascularization strategies carried increased early stroke risk compared with medical therapy alone—an important consideration given the asymptomatic population. For stenting, early procedural stroke and one perioperative death occurred; for endarterectomy, there were more early strokes than in the medical‑therapy group. These early hazards must be weighed against later reductions in ipsilateral stroke risk (for stenting) when counseling patients.
Interpretation and Clinical Implications
CREST‑2 provides contemporary randomized data comparing intensive modern medical management with revascularization plus intensive medical management in asymptomatic patients with high‑grade carotid stenosis. Key implications are:
- Modern intensive medical therapy produces low absolute ipsilateral stroke risks in asymptomatic high‑grade carotid stenosis, which narrows the margin for additional benefit from revascularization.
- Carotid‑artery stenting plus intensive medical care reduced the composite endpoint over 4 years compared with intensive medical care alone, despite higher early procedural risk—indicating a net benefit within the trial population over the observed follow‑up.
- Carotid endarterectomy plus intensive medical care did not show a statistically significant benefit over medical therapy alone in CREST‑2 during 4 years of follow‑up.
- Decision making should be individualized: clinicians must balance short‑term procedural risk, expected life expectancy, comorbidity burden, anatomic suitability, operator and institutional expertise, and patient preferences.
Expert Commentary, Limitations, and Areas for Caution
CREST‑2’s strengths include randomized, multicenter design, observer‑blinded outcome assessment, and use of a contemporary, aggressive medical regimen. Nevertheless, several caveats warrant emphasis:
- Population selection: CREST‑2 enrolled patients with ≥70% stenosis and without recent symptoms; results may not apply to lower‑grade stenosis or to patients with prior recent ipsilateral symptoms.
- Perioperative expertise: outcomes for stenting and endarterectomy are operator‑ and center‑dependent. Trial results reflect outcomes from participating sites and credentialed operators; community outcomes may differ.
- Follow‑up duration: the primary analysis reports outcomes up to 4 years. Longer follow‑up could modify absolute benefit estimates, especially if late procedural harms or late medical therapy effects emerge.
- Subgroup considerations: individual subgroups (e.g., age strata, sex, plaque morphology, contralateral occlusion) may experience different benefit–risk profiles; detailed subgroup analyses are important for clinical application.
Practical Recommendations for Clinicians
Based on CREST‑2 findings, clinicians should:
- Ensure that all patients with asymptomatic carotid stenosis receive intensive, guideline‑directed medical therapy as the foundation of care.
- Consider carotid‑artery stenting for selected patients with high‑grade asymptomatic stenosis who are informed about and accept the perioperative risk, have expected survival that justifies potential long‑term benefit, and are treated at centers with demonstrated expertise.
- Refrain from routine referral for carotid endarterectomy solely on the basis of asymptomatic high‑grade stenosis when optimized medical therapy is available, given the lack of a statistically significant benefit in CREST‑2; use individualized judgement for patients with specific anatomic or clinical indications.
- Engage in shared decision making, explicitly discussing early procedural risks, magnitude of absolute long‑term benefit, and the central role of intensive medical therapy.
Conclusion
CREST‑2 updates the evidence base for management of asymptomatic high‑grade carotid stenosis in the era of intensive medical therapy. Carotid‑artery stenting plus intensive medical management reduced the 4‑year incidence of perioperative stroke or death or subsequent ipsilateral ischemic stroke relative to intensive medical management alone; carotid endarterectomy did not show a significant advantage. These data support selective use of stenting in properly chosen patients treated in experienced centers, while underscoring the primacy of intensive medical prophylaxis and the need for careful, individualized decision making.
Funding and trial registration
CREST‑2 was funded by the National Institute of Neurological Disorders and Stroke and other sources. ClinicalTrials.gov identifier: NCT02089217.
References
1. Brott TG, Howard G, Lal BK, et al.; CREST‑2 Investigators. Medical Management and Revascularization for Asymptomatic Carotid Stenosis. N Engl J Med. 2025 Nov 21. doi:10.1056/NEJMoa2508800.
2. Endarterectomy for asymptomatic carotid artery stenosis. The ACAS (Asymptomatic Carotid Atherosclerosis Study) Collaborators. JAMA. 1995;273(18):1421–1428.
3. Halliday A, Harrison M, Hayter E, et al.; ACST Collaborative Group. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomized controlled trial. Lancet. 2004;363(9420):1491–1502.
4. Brott TG, Hobson RW 2nd, Howard G, et al.; CREST Investigators. Stenting versus endarterectomy for treatment of carotid‑artery stenosis. N Engl J Med. 2010;363(1):11–23.
5. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. (See subsequent updates for risk‑factor thresholds and secondary prevention strategies.)
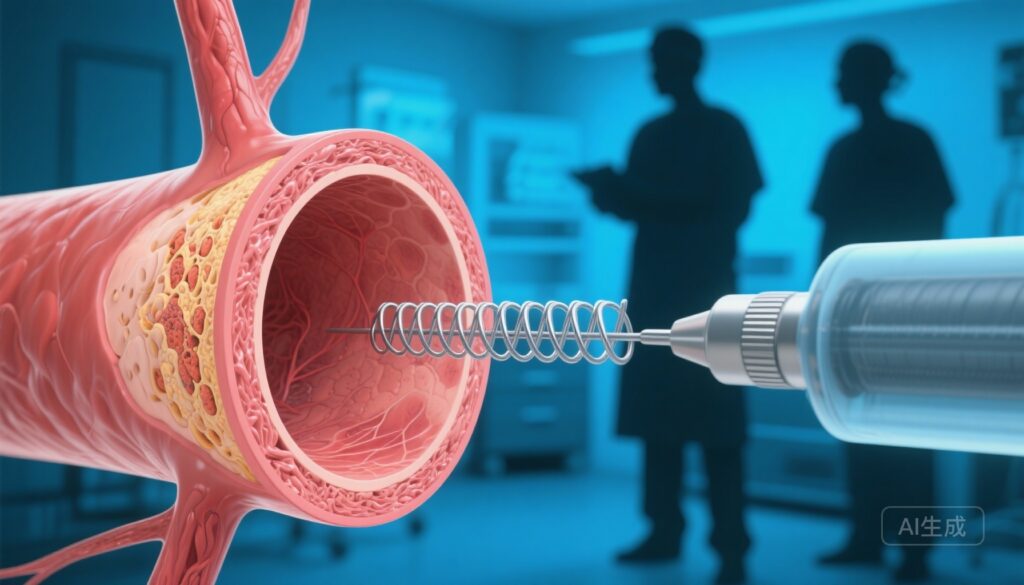
AI image prompt for article thumbnail
A polished, realistic medical illustration: cross‑section of the carotid bifurcation showing high‑grade atherosclerotic plaque on one side; on the other side a metallic carotid stent being deployed with small catheter visible; subtle silhouettes of a vascular surgeon and interventionalist consulting in background; cool clinical blues and neutral tones; high detail, 3:2 aspect ratio.