Study Background and Disease Burden
Neoatherosclerosis is a recognized pathological process characterized by the development of atherosclerotic changes within the neointima of previously implanted stents, leading to late stent failure beyond one year after drug-eluting stent (DES) implantation. It represents a critical clinical challenge, particularly following primary percutaneous coronary intervention (pPCI) used to treat ST-segment elevation myocardial infarction (STEMI). Despite the advancement in DES technology—specifically the use of everolimus-eluting stents (EES)—neoatherosclerosis remains an important contributor to adverse late clinical events, including restenosis and late stent thrombosis.
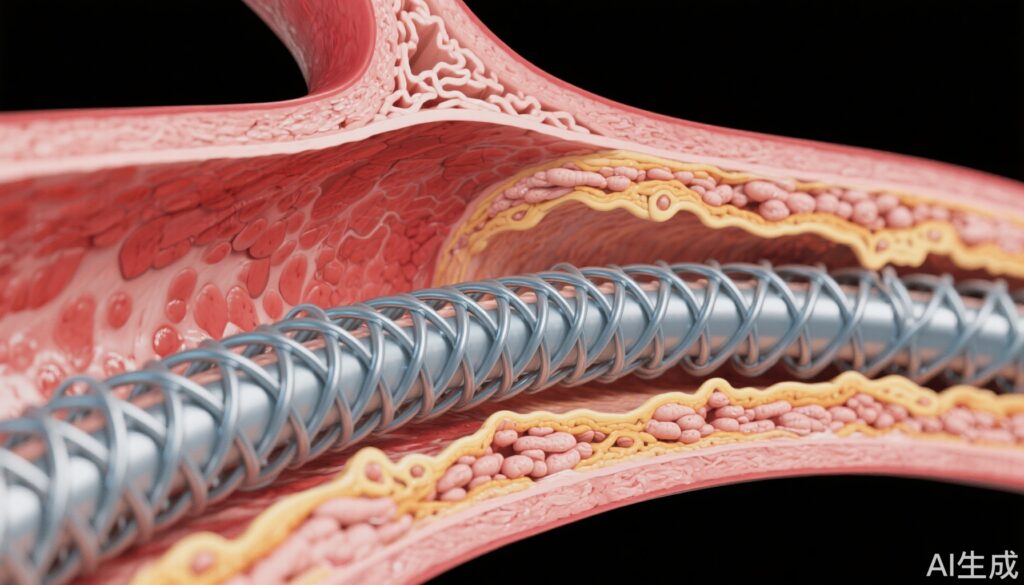
Drug-eluting stents have evolved with the introduction of different polymer coatings. Durable polymers (DP), which permanently coat the stent, are associated with prolonged inflammatory responses due to their permanence, potentially fostering neoatherosclerosis development. Biodegradable polymers (BP) aim to reduce this risk by degrading over time, thereby minimizing chronic vessel wall irritation. However, an unsettled question remains regarding whether BP-EES confer a significant long-term advantage in reducing neoatherosclerosis over DP-EES, especially in the acute STEMI setting, where inflammatory and healing responses may be heightened.
Given the significant morbidity associated with late stent failure in STEMI patients, clarifying whether BP stents truly mitigate the risk of neoatherosclerosis compared to DP stents was the primary motivation for the CONNECT trial.
Study Design
The CONNECT trial (NCT03440801) was a randomized, controlled, multicenter clinical study conducted across institutions in Japan and Switzerland. It enrolled a total of 239 patients presenting with STEMI who underwent primary PCI. Participants were randomized in a 1:1 ratio to receive either a biodegradable polymer everolimus-eluting stent (BP-EES) or a durable polymer everolimus-eluting stent (DP-EES).
The primary endpoint was the frequency of neoatherosclerosis assessed 3 years post-implantation using high-resolution optical coherence tomography (OCT). Neoatherosclerosis was stringently defined as the presence of fibroatheroma, fibrocalcific plaque, or macrophage accumulation within the neointimal tissue of the stent. Secondary endpoints included the frequency of specific pathological subtypes of neoatherosclerosis and clinical outcomes such as target lesion failure (TLF).
Key Findings
Out of 239 randomized patients, 236 successfully underwent stenting (119 BP-EES and 117 DP-EES). Of those, 178 patients (75%) completed the 3-year OCT assessment (88 in the BP-EES group and 90 in the DP-EES group), allowing for robust comparison.
The incidence of neoatherosclerosis at 3 years was similar between groups: 11.4% in the BP-EES cohort and 13.3% with DP-EES (odds ratio 0.83; 95% confidence interval 0.33 to 2.04; P = .69). No statistically significant difference emerged in the presence of fibroatheromas (BP-EES 9.1% vs. DP-EES 11.1%, P = .66) or macrophage infiltration (BP-EES 4.5% vs. DP-EES 3.3%, P = .68). Notably, no fibrocalcific neoatherosclerosis was detected in either study arm.
In clinical terms, target lesion failure rates were nearly identical between the groups (BP-EES 5.9% vs. DP-EES 6.0%, P = .97), indicating that the polymer type did not significantly influence major adverse cardiac events over the 3-year follow-up.
These findings suggest equipoise in long-term vascular healing and inflammatory response between BP-EES and DP-EES in the STEMI population. The anticipated benefit of biodegradable polymers in reducing neoatherosclerosis risk was not realized in this carefully controlled clinical setting.
Expert Commentary
This landmark investigation challenges the previously held hypothesis that biodegradable polymer technology inherently reduces the long-term incidence of neoatherosclerosis. While biodegradable polymers were theorized to elicit less chronic inflammation by dissolving after drug elution, the CONNECT trial’s three-year data imply comparable vascular responses with current-generation durable polymer stents.
One must consider the sophisticated design and sensitivity of OCT imaging as a strength in detecting subtle differences, adding confidence to the negative result. However, it also raises questions about whether mechanisms beyond polymer biodegradability—such as strut thickness, drug kinetics, or patient-specific inflammatory milieu—may play critical roles in neoatherosclerosis development.
Additionally, the similar target lesion failure rates reinforce that clinical decision-making can incorporate either stent type without compromising medium-term outcomes in STEMI patients.
Limitations to acknowledge include the study’s relatively modest sample size and the follow-up period limited to three years, which may not capture very late stent failures or the complete natural history of neoatherosclerosis progression. The majority of patients hailed from Japan and Switzerland; hence, extrapolation to more diverse populations requires caution.
Conclusion
The CONNECT trial demonstrates that, at three years post-primary PCI in STEMI patients, biodegradable polymer everolimus-eluting stents do not confer superiority over durable polymer EES regarding neoatherosclerosis frequency or clinical outcomes. This evidence suggests that the choice between BP-EES and DP-EES should be individualized based on other clinical considerations rather than presumed long-term advantages in neoatherosclerosis prevention.
Further studies with extended follow-up and broader populations are warranted to conclusively define the role of stent polymer composition in late vascular healing and stent durability.
References
Taniwaki M, Häner JD, Kakizaki R, Ohno Y, Yahagi K, Higuchi Y, et al. Long-term effect of biodegradable vs. durable polymer everolimus-eluting stents on neoatherosclerosis in ST-segment elevation myocardial infarction: the CONNECT trial. Eur Heart J. 2025 Aug 1;46(29):2906-2916. doi: 10.1093/eurheartj/ehae589. PMID: 39217617.