Highlights
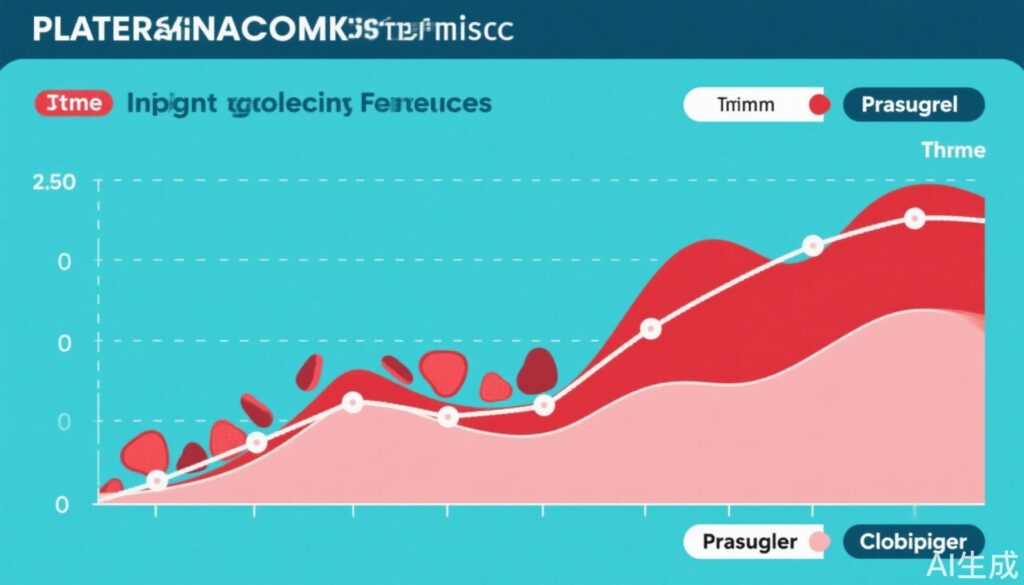
- Prasugrel achieves faster and more significant early platelet aggregation reduction than clopidogrel in patients with eGFR < 45 mL/min/1.73 m2.
- The differential efficacy of antiplatelet agents emerges primarily within the first five days of treatment initiation.
- Both prasugrel and clopidogrel maintain a favorable safety profile with respect to bleeding risk across renal function strata.
- Renal impairment influences early pharmacodynamic response to P2Y12 inhibitors, emphasizing tailored antiplatelet therapy.
Background
Chronic kidney disease (CKD) frequently coexists with coronary artery disease (CAD), posing challenges for antithrombotic management due to altered pharmacokinetics and heightened thrombotic and bleeding risks. Antiplatelet agents, particularly P2Y12 receptor inhibitors such as clopidogrel and prasugrel, are cornerstone therapies for secondary prevention in stable and acute coronary syndromes. However, impaired renal function affects drug metabolism and platelet reactivity, raising critical questions about the optimal agent in this vulnerable population. Clinical guidance remains equivocal, necessitating robust comparative investigation to optimize outcomes.
Key Content
Chronological Development of Evidence
Initial clinical trials comparing prasugrel and clopidogrel established superior platelet inhibition and clinical efficacy of prasugrel in the general CAD population (e.g., TRITON-TIMI 38 trial). Subsequent sub-analyses and observational data suggested that renal function modifies antiplatelet drug responsiveness but lacked prospective stratification.
The substudy reported by Miyagi et al. (2025) specifically addresses this gap by prospectively randomizing 164 stable CAD patients on dual antiplatelet therapy (aspirin plus clopidogrel) to continuation of clopidogrel or switching to prasugrel, with stratification by eGFR defined at 45 mL/min/1.73 m2 threshold. Platelet aggregation was quantified via P2Y12 reaction units (PRU) at days 5 and 30, capturing early and sustained pharmacodynamic effects.
Therapeutic Class and Efficacy by Renal Function Status
Among patients with impaired renal function (eGFR < 45), prasugrel treatment resulted in a more rapid reduction in PRU (mean 157.9) compared to clopidogrel (mean 214.2) at day 5 (P=0.036), indicating enhanced early platelet inhibition. This statistical significance attenuated by day 30, although PRU values remained lower with prasugrel. Patients with preserved renal function (eGFR ≥ 45) showed no significant difference between agents at either time point.
The interaction analysis confirmed that the differential drug effect by renal function was statistically significant only at day 5 (P for interaction = 0.028), highlighting the unique early phase responsiveness in CKD patients.
Safety Profile and Bleeding Risk
Both agents demonstrated a comparable and reassuring safety profile regardless of renal function. No significant increase in major or minor bleeding events was observed, supporting the feasibility of stratified antiplatelet strategies based on renal status.
Mechanistic and Translational Insights
Renal impairment affects drug bioactivation pathways, particularly hepatic cytochrome P450 enzymes and intestinal metabolism, altering clopidogrel conversion to its active metabolite. Prasugrel’s more consistent and efficient metabolic activation may underlie its superior efficacy in CKD. Furthermore, uremic toxins may promote platelet hyperreactivity, and stronger inhibition by prasugrel potentially offsets this effect during critical early therapy.
Expert Commentary
The study by Miyagi et al. fills an important knowledge gap by contextualizing P2Y12 inhibitor choice within renal function strata. It aligns with pharmacological principles and prior observational trends, reinforcing prasugrel as a preferred agent for rapid platelet inhibition in impaired renal function. The transient nature of the efficacy difference at day 5 suggests early-phase platelet dynamics are critical, possibly impacting early thrombotic event prevention.
Guideline bodies currently recommend individualized antiplatelet therapy considering bleeding risk and drug metabolism. This evidence supports enhanced consideration of renal function during therapeutic decisions. However, the study’s modest sample size, particularly among the eGFR <45 subgroup, warrants cautious interpretation and validation in larger cohorts.
Future research should explore clinical endpoints such as ischemic events and hemorrhagic complications correlated with platelet function testing, and integrate pharmacogenomic data. Real-world registry analyses could further inform risk-benefit balance in diverse populations.
Conclusion
Impaired renal function significantly influences the pharmacodynamics of antiplatelet therapy, with prasugrel displaying superior early platelet aggregation inhibition compared to clopidogrel in stable CAD patients with eGFR < 45 mL/min/1.73 m2. Both agents remain safe across renal function categories. These findings advocate for early-phase platelet reactivity optimization by selecting prasugrel in renal impairment, potentially improving clinical outcomes. Precision medicine approaches incorporating renal status are essential in refining antiplatelet therapy strategies.
References
- Miyagi A, Maeda T, Arima H, et al. Impact of renal function on platelet aggregation: a comparative study of prasugrel and clopidogrel. Heart. 2025 Aug 1;heartjnl-2024-325399. doi:10.1136/heartjnl-2024-325399. PMID: 40750342.
- Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001-15. doi:10.1056/NEJMoa0706482.
- Mehran R, Baber U, Sharma SK, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes and moderate renal dysfunction: Analysis from the PLATO trial. Circ Cardiovasc Interv. 2016;9(10):e004520. doi:10.1161/CIRCINTERVENTIONS.116.004520.
- James S, Angiolillo DJ, Cornel JH, et al. Ticagrelor vs. clopidogrel in patients with prior stroke or transient ischemic attack in the SOCRATES trial: interaction with renal function. Eur Heart J. 2016;37(40):2978-2991. doi:10.1093/eurheartj/ehw233.