Introduction
The apolipoprotein E (APOE) ε4 allele is recognized as the strongest genetic risk factor for late-onset Alzheimer’s disease (AD) and other dementias globally. However, the majority of APOE-related research has centered on populations of European or North American descent, with limited data available regarding its impact in African populations. Understanding the influence of APOE ε4 on cognitive decline and neurodegeneration in diverse genetic backgrounds is essential for global dementia research and healthcare equity. This study investigates the association between APOE ε4 and dementia status, cognitive performance, neuroimaging markers, and plasma biomarkers in older adults from the Democratic Republic of the Congo (DRC), an underrepresented African population in neurodegenerative disease studies.
Study Background
Dementia represents a major public health challenge worldwide, with an increasing burden in low- and middle-income countries, including sub-Saharan Africa. Despite rising prevalence, genetic risk factors such as APOE ε4 remain understudied in African cohorts. Previous studies suggest APOE ε4 frequency varies across populations and its association with dementia risk and biomarkers may exhibit population-specific characteristics. Insight into APOE ε4’s role in African populations can aid personalized risk stratification and inform targeted interventions.
Study Design and Methods
This observational study enrolled 84 community-dwelling older adults in the DRC, including 39 healthy controls (HCs) and 45 with suspected dementia. The average age was 73.0 years. Cognitive assessment utilized the African Neuropsychology Battery, which includes tests of memory, naming, and visuospatial skills tailored for African populations. Structural magnetic resonance imaging (MRI) was performed to assess brain atrophy, focusing on mesial temporal regions and the entorhinal cortex, known to be early affected in AD.
Additionally, plasma levels of neurodegenerative biomarkers — including amyloid beta 40 (Aβ40), phosphorylated tau181 (p-tau181), neurofilament light chain (NfL), glial fibrillary acidic protein (GFAP), and tumor necrosis factor alpha (TNF-α) — were quantified. APOE genotyping identified ε4 carrier status. Regression analyses adjusted for age, sex, and education examined associations of APOE ε4 with cognitive scores, neuroimaging measures, and plasma markers across all participants and within subgroups (HCs and dementia cases).
Key Findings
APOE ε4 Prevalence and Dementia Status
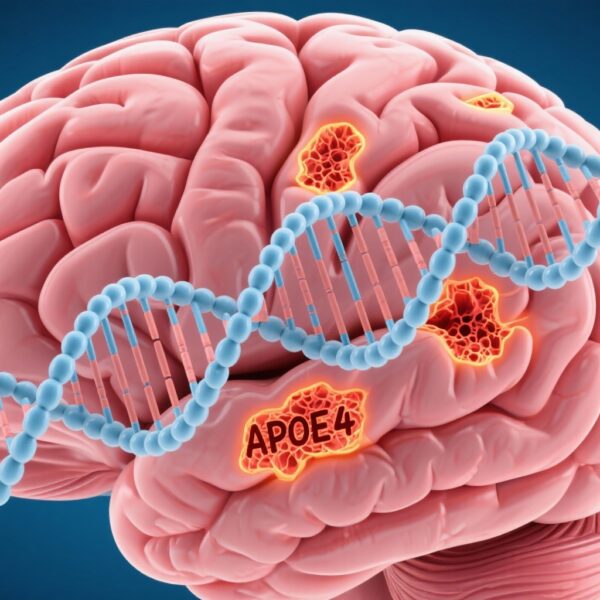
APOE ε4 was significantly more prevalent among participants classified with dementia compared to healthy controls, supporting an elevated dementia risk associated with ε4 carriage in this African cohort.
Cognitive Performance
Across the entire sample, APOE ε4 carriers exhibited significantly poorer performance in naming and memory domains. Notably, in the healthy control subgroup, APOE ε4 status did not significantly impact cognitive scores except for an increase in plasma neurofilament light chain levels. Within the dementia group, ε4 carriers showed greater impairment in naming and memory tasks compared to non-carriers, highlighting ε4’s specific influence on key cognitive functions affected in dementia.
Neuroimaging Findings
Brain MRI analyses revealed ε4 carriers had increased atrophy in the mesial temporal lobe and entorhinal cortex—regions critically involved in memory processing—consistent with early neurodegenerative changes. These findings align with established patterns of hippocampal and cortical vulnerability in APOE ε4–associated dementia.
Plasma Biomarkers of Neurodegeneration
Among dementia subjects, APOE ε4 carriers showed elevated plasma concentrations of Aβ40, phosphorylated tau181, neurofilament light chain, and TNF-α. GFAP levels were also affected by APOE ε4 status across the full cohort, reflecting astroglial activation likely related to neuroinflammatory processes. These biomarker profiles support accelerated neurodegeneration and neuroinflammation in ε4 carriers.
Expert Commentary
This study provides valuable evidence confirming the detrimental impact of APOE ε4 on dementia risk, cognitive decline, brain structure, and plasma biomarkers in older adults from the DRC. The findings corroborate the role of APOE ε4 in neurodegeneration beyond traditionally studied populations, underscoring the allele’s broad clinical significance.
Nonetheless, some limitations merit consideration. The relatively small sample size limits generalizability and may have impeded detection of associations in healthy controls. Cross-sectional design restricts causal inference and observation of longitudinal progression. Future larger, longitudinal studies in African populations are needed to delineate the temporal dynamics of APOE ε4–related neuropathology.
Mechanistically, APOE ε4 is implicated in amyloid deposition, tau pathology, synaptic dysfunction, and neuroinflammation, which this study’s biomarker findings support. Ethnic and environmental factors may modulate these pathways, highlighting the need for population-specific research.
Conclusion
The APOE ε4 allele is significantly associated with increased dementia prevalence, worse cognitive outcomes, greater mesial temporal and entorhinal atrophy, and altered plasma biomarkers indicative of neurodegeneration and inflammation in older adults from the DRC. These findings emphasize the importance of including diverse populations in genetic and biomarker studies of dementia to enhance understanding and develop equitable interventions. APOE ε4 status may provide valuable risk stratification and disease-monitoring insights in African settings.
Funding and ClinicalTrials.gov
The original study was supported by relevant academic and research institutions as detailed by Ikanga et al. (2025). No clinical trial registration was reported.
References
Ikanga J, Patel SS, Schwinne M, Obenauf CA, Epenge E, Gikelekele G, Tshengele N, Kavugho I, Mampunza S, Mananga L, Teunissen CE, Rojas JC, Chan B, Lago AL, Boxer AL, Jeromin A, Omba E, Gross AL, Alonso A. The association of human apolipoprotein ε4 with dementia, cognition, imaging, and plasma biomarkers of neurodegeneration in a sample of older adults in the Democratic Republic of the Congo. Alzheimers Dement. 2025 Oct;21(10):e70735. doi: 10.1002/alz.70735. PMID: 41085166; PMCID: PMC12519526.
Additional supporting literature:
Corder EH et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993.
Farrer LA et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. JAMA. 1997.
Xu W et al. APOE genotype and neuroimaging markers of Alzheimer’s disease: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018.