Highlights
– Antimicrobial resistance (AMR) among ESKAPE pathogens drives significant increases in hospital costs and length of stay (LOS) in Vietnam.
– Carbapenem-resistant Acinetobacter baumannii (CRAB) is associated with the highest incremental cost and LOS.
– The cost gap between resistant and susceptible infections widened during the COVID-19 pandemic.
– MRSA was the only pathogen where resistance did not lead to higher costs.
Study Background and Disease Burden
Antimicrobial resistance (AMR) is a mounting global health issue, particularly acute in low- and lower-middle-income countries (LMICs), where healthcare infrastructure and resource allocation are already strained. The ESKAPE group—comprising Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species—remains central to hospital-acquired infections and is prioritized by the World Health Organization (WHO) due to their high resistance rates and impact on clinical outcomes. Despite this, robust data quantifying the hospital economic burden of AMR among ESKAPE pathogens in LMIC settings have been limited. The COVID-19 pandemic has further complicated resource allocation, highlighting the need for contemporary, context-specific evidence to guide healthcare investment and stewardship efforts.
Study Design
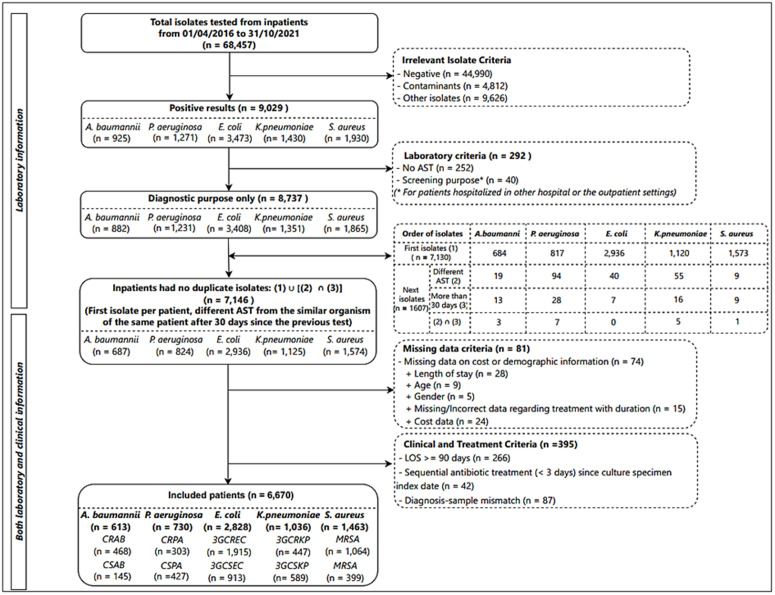
This retrospective observational study analyzed healthcare utilization at the Hospital for Tropical Diseases, a major tertiary referral center in Vietnam, from 2016 to 2021. Eligible participants were patients with non-duplicate clinical isolates of any ESKAPE pathogen. Pathogens were classified as resistant or susceptible based on WHO guidelines. Incremental hospital costs and LOS attributable to AMR were estimated using multivariate generalized linear regression (for costs) and negative binomial regression (for LOS), including a linear spline for COVID-19 onset in 2020. Sociodemographic and clinical covariates were included to adjust for confounding factors. Difference-in-difference (DiD) methodology was applied to quantify the change in cost gap between resistant and susceptible cases pre- and post-COVID-19.
Key Findings
A total of 6,670 patients were included, with 4,197 (62.92%) having ESKAPE pathogens isolated. The most prevalent priority pathogens were third-generation cephalosporin-resistant Escherichia coli (3GCREC, 45.63%) and methicillin-resistant Staphylococcus aureus (MRSA, 25.33%).
After adjusting for covariates, the incremental hospital costs per patient with a resistant isolate were markedly higher for most pathogens:
– CRAB: $3,980
– CRPA (Carbapenem-resistant Pseudomonas aeruginosa): $1,000
– 3GCREC: $444
– 3GCRKP (Third-generation cephalosporin-resistant Klebsiella pneumoniae): $1,942
– MRSA: -$326 (not statistically significant)
Incremental LOS also varied substantially by pathogen:
– 3GCREC: 1.40 days (95% CI: 0.69-2.10)
– CRPA: 12.54 days (95% CI: 11.12-13.97)
COVID-19 emerged as a major modifier of healthcare utilization. The cost gap between resistant and susceptible cases widened significantly post-pandemic, with the most pronounced difference observed for CRAB ($9,116, 95% CI: $6,019-$12,213, DiD analysis).
Expert Commentary
These findings offer robust, methodologically sound evidence of the substantial economic impact imposed by AMR in a high-burden LMIC setting. The cost and LOS increments align with international observations but are amplified in Vietnam, likely due to limited access to advanced therapeutics and infection control resources. Notably, MRSA did not drive higher costs, possibly reflecting local treatment protocols or early identification practices unique to the study site.
The COVID-19 pandemic exacerbated cost disparities, likely due to increased case complexity, supply chain disruptions, and heightened infection control measures. These results underscore the urgency for targeted interventions—such as enhanced stewardship, infection prevention, and rapid diagnostics—to mitigate the resource drain from AMR, especially in post-pandemic recovery planning.
Limitations include the single-center design, which may limit generalizability, and possible unmeasured confounders (e.g., severity of illness, comorbidity profiles). However, the rigorous adjustment for sociodemographic and clinical variables lends credibility to the observed associations.
Conclusion
AMR among ESKAPE pathogens substantially increases hospital costs and LOS in Vietnam, with carbapenem-resistant A. baumannii imposing the greatest burden. The COVID-19 pandemic has further widened the gap between resistant and susceptible infections, highlighting the need for focused investment in AMR prevention and control. Future research should expand to multi-center settings and explore the impact of stewardship interventions on cost and clinical outcomes.
References
Nguyen NT, Nguyen NP, Truong QT, Huynh TP, Tran-Thi HN, Hoang MV, Nguyen-Thi HY. Healthcare utilization associated with antimicrobial resistance at a tertiary hospital in Vietnam: A retrospective observational study from 2016 to 2021. PLoS One. 2025 Aug 4;20(8):e0329539. doi: 10.1371/journal.pone.0329539 IF: 2.6 Q2 . PMID: 40758725 IF: 2.6 Q2 ; PMCID: PMC12321119 IF: 2.6 Q2 .