Highlights
- The AlphaBet interim analysis reports that combined 177Lu‑PSMA‑I&T (7.4 GBq) plus radium‑223 (recommended 55.0 kBq/kg) administered every 6 weeks is feasible and well tolerated in selected patients with metastatic castration‑resistant prostate cancer (mCRPC) with bone metastases.
- No dose‑limiting toxicities were observed. PSA decline ≥50% occurred in 55% (18/33) of evaluable patients (95% CI 36–72).
- Grade ≥3 treatment‑related hematologic events were uncommon (14% overall), supporting further study of combined α and β approaches, with attention to marrow toxicity and bone health management.
Background and clinical context
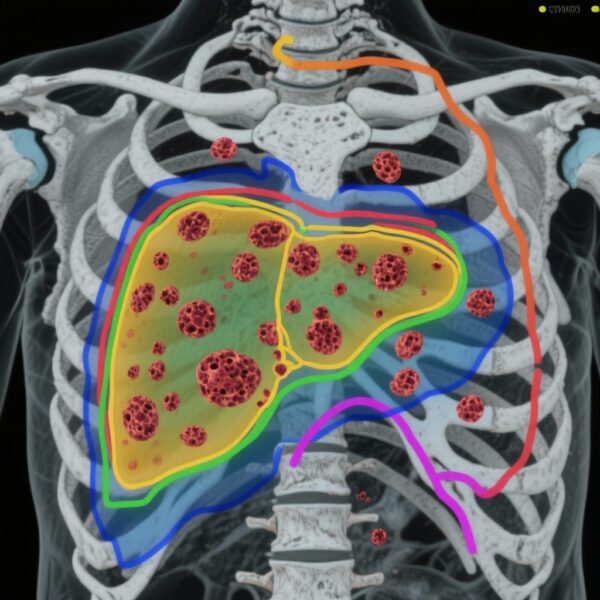
Prostate cancer remains a leading cause of cancer morbidity and mortality worldwide. For men with metastatic castration‑resistant prostate cancer (mCRPC), life‑prolonging systemic options now include androgen receptor pathway inhibitors, chemotherapy, and molecular radioligand therapies that target prostate‑specific membrane antigen (PSMA). Two radiopharmaceutical strategies have demonstrated survival benefits in mCRPC with bone‑predominant disease: beta‑particle emitting 177Lu‑labelled PSMA ligands and the bone‑seeking alpha emitter radium‑223 dichloride. Each modality has distinct physical properties and tissue effects: 177Lu delivers relatively longer‑range beta radiation favoring soft‑tissue and mixed bone disease control, whereas radium‑223 emits short‑range α particles with high linear energy transfer, preferentially affecting bone microenvironment and causing potent local cytotoxicity.
Despite these advances, resistance to single‑agent radioligand therapy is common and median durations of benefit are finite. Combining α and β radiopharmaceuticals is a biologically plausible strategy to broaden cytotoxic coverage (bone niche and PSMA‑expressing soft tissue), potentially overcome heterogeneous disease, and improve disease control. However, overlapping marrow toxicity is a critical safety consideration that warrants careful dose‑finding.
Study design
The AlphaBet trial is an investigator‑initiated, single‑centre, single‑arm phase 1/2 study conducted at the Peter MacCallum Cancer Centre (Melbourne, Australia; ClinicalTrials.gov NCT05383079). Key eligibility criteria included adult patients (≥18 years) with progressive mCRPC, ECOG 0–2, at least two untreated visible bone metastases, prior exposure to an androgen receptor pathway inhibitor, and strict imaging selection: PSMA‑positive disease defined by a maximum standardized uptake value (SUVmax) ≥20 at a disease site and absence of discordant sites (no lesions with high FDG uptake and low PSMA expression or lesions not visible on bone scintigraphy).
Phase 1 employed dose‑escalation of radium‑223 at two predefined dose levels (27.5 kBq/kg and 55.0 kBq/kg) combined with fixed 7.4 GBq 177Lu‑PSMA‑I&T, administered intravenously every 6 weeks for up to six cycles. Co‑primary endpoints were the maximum tolerated or administered dose and the recommended phase 2 dose (phase 1), and the prostate‑specific antigen (PSA) response rate (≥50% decline from baseline; phase 2). Safety was assessed in all treated patients and activity in those treated at the recommended dose.
An amendment added a planned interim analysis; results reported here correspond to that interim analysis (enrolment Nov 3, 2022–Nov 5, 2024).
Key findings
Patient population and treatment exposure
Thirty‑seven patients were enrolled; 36 (97%) received at least one dose and were included in the safety analysis (median age 72.5 years, IQR 67–78). Thirty‑three (89%) were included in the preliminary activity analysis. Median follow‑up was 13.3 months (IQR 8.7–17.1). Eleven patients (31%) completed all six cycles of both agents, while 18 (50%) discontinued early—most commonly for unequivocal disease progression (61% of discontinuations) or adverse events (17%).
Dose escalation and recommended dose
No dose‑limiting toxicities (DLTs) were observed in the escalation cohorts. The recommended phase 2 radium‑223 dose when combined with 7.4 GBq 177Lu‑PSMA‑I&T every 6 weeks was 55.0 kBq/kg.
Antitumour activity
Among 33 evaluable patients treated at the maximum tolerated/administered dose, a PSA decline of ≥50% from baseline (PSA50) was observed in 18 patients (55%; 95% CI 36–72). This is an encouraging signal of preliminary activity in a cohort selected for high PSMA expression.
Safety
Overall, the combination showed an acceptable acute safety profile. Grade 3 or higher treatment‑related adverse events (TRAEs) occurred in five of 36 patients (14%), comprising anaemia (4 patients, 11%) and neutropenia (3 patients, 8%). No treatment‑related deaths were reported. Non‑clinically significant grade 3 lymphopenia occurred in 10 patients (28%). The observed hematologic toxicity rates are consistent with anticipated marrow effects from systemic radiotherapy but not excessive in this selected cohort.
Other observations
Treatment discontinuations were mostly driven by disease progression rather than tolerability. The trial used stringent imaging selection (SUVmax ≥20 and exclusion of discordant FDG‑avid/low‑PSMA lesions), which likely enriched for PSMA‑avid, radioligand‑responsive patients and may have influenced response rates.
Expert commentary: interpretation, strengths, and limitations
Interpretation
AlphaBet provides the first prospective evidence that combining a beta‑particle PSMA radioligand (177Lu‑PSMA‑I&T) with an alpha‑emitting, bone‑targeting radiopharmaceutical (radium‑223) is feasible and can be administered safely at the tested dose levels in a selected mCRPC population. The PSA50 rate of 55% in this cohort is encouraging and supports biological plausibility for enhanced disease control when pairing bone‑targeted α therapy with PSMA‑directed β therapy.
Strengths
– Rational biological strategy: The two agents have complementary physical properties and target different compartments of metastatic disease (PSMA‑expressing soft tissue and osteoblastic bone microenvironments).
– Careful dose escalation with predefined safety endpoints and a conservative treatment schedule (every 6 weeks) minimized immediate toxicity concerns.
– Stringent imaging‑based selection reduced heterogeneity and enriched for PSMA‑avid disease, increasing the interpretability of early activity signals.
Limitations and caveats
– Single‑centre, single‑arm design: Without a randomized comparator, it is not possible to quantify the incremental benefit of adding radium‑223 to 177Lu‑PSMA‑I&T versus 177Lu‑PSMA monotherapy or standard systemic care.
– Small sample size and interim nature: Confidence intervals around activity estimates are wide and follow‑up remains limited for durability and survival endpoints.
– Selection bias: The SUVmax ≥20 threshold is stringent and may not reflect patients encountered in routine practice, limiting generalizability.
– Bone health and prior safety signals: Combinations involving radium‑223 have previously prompted caution regarding fracture risk when combined with certain systemic agents, underscoring the need for proactive bone protective strategies (e.g., bisphosphonates or denosumab) and fracture surveillance when combining therapies that affect bone health and marrow reserve.
– Long‑term marrow toxicity: The cumulative marrow impact of combined α and β therapies over time requires longer follow‑up and careful hematologic monitoring, particularly for late cytopenias or secondary hematologic malignancies.
Implications for practice and research
The AlphaBet interim data provide a rationale to pursue randomized trials comparing combination α+β radiopharmaceutical therapy to 177Lu‑PSMA alone or to other standard‑of‑care options. Key design considerations for future trials include stratification for prior therapies, incorporation of bone health measures (baseline DEXA, prophylactic bone‑protecting agents), comprehensive hematologic monitoring, endpoints beyond PSA (radiographic progression‑free survival, symptomatic skeletal events, overall survival), and inclusion of patient‑reported outcomes to capture pain and functional benefits relevant to bone‑predominant disease.
Mechanistic and biomarker directions
Exploration of predictive biomarkers will be critical. While high PSMA uptake predicts PSMA‑directed activity, optimal thresholds and alternative biomarkers (molecular characterization of tumour clones, circulating tumour DNA, or bone microenvironment markers) may refine patient selection for combination approaches. Dosimetry studies could clarify optimal scheduling and individualized dosing to maximize tumouricidal effect while minimizing marrow exposure.
Conclusion and next steps
The AlphaBet phase 1/2 interim analysis shows that combining 177Lu‑PSMA‑I&T with radium‑223 at the tested doses is feasible and demonstrates encouraging preliminary antitumour activity with manageable acute hematologic toxicity in a carefully selected mCRPC population. These data justify further evaluation in larger, preferably randomized studies with longer follow‑up and comprehensive safety monitoring. Future trials should prioritize clinically meaningful endpoints (radiographic PFS, symptomatic skeletal events, overall survival), bone health interventions, and correlative studies to optimize patient selection and dosing strategies.
Funding and trial registration
The AlphaBet trial was supported by the Prostate Cancer Foundation, Bayer, and the National Health and Medical Research Council. The trial is registered at ClinicalTrials.gov (NCT05383079).
Selected references
1. Kostos L, Buteau JP, Xie J, et al. Lutetium‑177 [177Lu]Lu‑PSMA‑I&T plus radium‑223 in patients with metastatic castration‑resistant prostate cancer (AlphaBet): an interim analysis of the investigator‑initiated, single‑centre, single‑arm, phase 1/2 trial. Lancet Oncology. 2025 Nov;26(11):1479–1488. doi:10.1016/S1470-2045(25)00559-5.
2. Parker C, Nilsson S, Heinrich D, et al. Alpha emitter radium‑223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213–223. (ALSYMPCA trial)
Note: This article summarizes interim results and contextual considerations. Clinicians should consult the full AlphaBet publication and regulatory guidance before applying these findings in practice.