Highlight
- This randomized clinical trial is the first to rigorously assess whether PPV23 reduces major cardiovascular events in at-risk adults without prior cardiovascular disease.
- Over a median of 7 years, PPV23 vaccination did not significantly reduce fatal or nonfatal acute coronary syndrome or ischemic stroke compared to placebo.
- The study was limited by a lower than expected event rate, reducing statistical power to detect moderate treatment effects.
- Exploratory analyses showed no benefit on all-cause mortality, hospital presentations, or cardiovascular procedures.
Study Background and Disease Burden
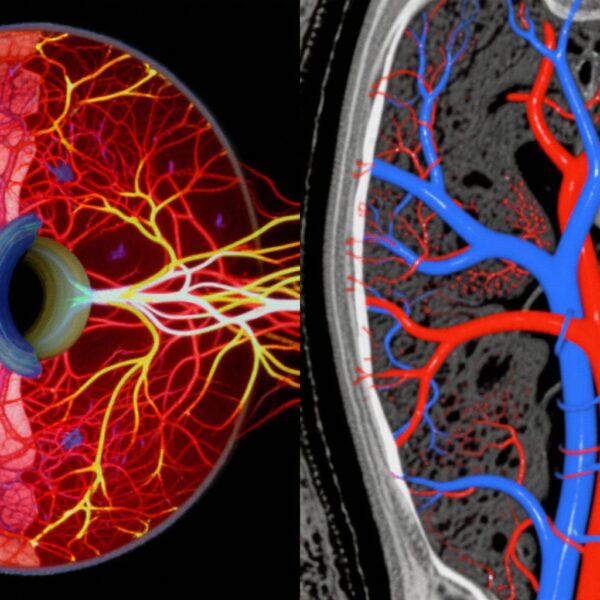
Cardiovascular disease (CVD) remains the leading cause of morbidity and mortality globally. Acute coronary syndrome (ACS) and ischemic stroke represent major contributors to cardiovascular-related deaths and disability. Preventive strategies focus on controlling traditional risk factors such as hypertension, hypercholesterolemia, obesity, diabetes, and smoking.
Intriguingly, evidence from animal models and meta-analyses of observational human data suggested that pneumococcal polysaccharide vaccination (PPV), primarily used to prevent pneumococcal infection, may have a protective effect against atherosclerosis, the underlying pathology of many cardiovascular events. Proposed mechanisms include reduction in systemic inflammation and cross-reactive immune responses that attenuate atherogenesis.
Despite these experimental and observational findings, no randomized clinical trial had evaluated whether PPV could reduce major cardiovascular events in humans. This unmet clinical question motivated the current study.
Study Design
The Prevention of Adverse Cardiovascular Events Using the 23-Valent Pneumococcal Polysaccharide Vaccine trial was a double-blind, placebo-controlled, parallel-group randomized clinical trial. Conducted at six Australian centers from 2016 to 2017, the study enrolled 4725 community-dwelling adults aged 55 to 60 years who had at least two cardiovascular risk factors (obesity, hypertension, or hypercholesterolemia) but no previous cardiovascular events or specific indications for early pneumococcal vaccination.
Participants were randomized to receive either the 23-valent pneumococcal polysaccharide vaccine (PPV23; Pneumovax by Merck Sharp & Dohme Corp) or a placebo (saline injection). The primary composite outcome was fatal or nonfatal acute coronary syndrome (including myocardial infarction) or ischemic stroke. Outcomes were ascertained through comprehensive electronic medical records using ICD-10-AM codes over a mean follow-up period of 7 years.
Analyses were conducted using competing risk proportional hazards regression models, stratified by sex and study center.
Key Findings
Of the 4725 randomized participants (52% male; mean age 58.0 years), 2366 were assigned to PPV23 and 2357 to placebo. There was no statistically significant difference in the primary composite outcome—58 events occurred in the PPV group versus 64 in the placebo group (hazard ratio [HR] 0.90; 95% confidence interval [CI], 0.63 to 1.28; P = .57).
Secondary/exploratory outcomes including all-cause mortality, all-cause hospital presentations, and cardiovascular-related hospital procedures likewise showed no meaningful differences between groups.
Notably, the event rate was lower than anticipated, which limited the statistical power to detect modest treatment effects. Consequently, while the point estimate slightly favored the vaccine, the confidence intervals were wide and include the possibility of no effect or modest benefit.
Expert Commentary
This landmark randomized clinical trial provides the first high-quality evidence that PPV23 vaccination does not confer significant protection against major cardiovascular events in individuals at intermediate cardiovascular risk without prior events.
The study’s strengths include robust randomized, double-blind design, long-term follow-up, comprehensive electronic health record-based outcome ascertainment, and stratified analysis.
Limitations center on the unexpectedly low incidence of cardiovascular outcomes in the cohort, which diminished statistical power. It remains possible that benefits might emerge in higher-risk patients or with alternative vaccination schedules such as conjugate pneumococcal vaccines that elicit different immunological profiles.
Current guidelines do not recommend pneumococcal vaccines for primary cardiovascular prevention. These findings suggest that routine PPV23 vaccination should not be considered a strategy to reduce cardiovascular events in this population. Mechanistic insights suggest the previously postulated anti-atherogenic effects are either minimal in humans or require additional immunomodulatory interventions.
Conclusion
This rigorous randomized clinical trial demonstrates that the 23-valent pneumococcal polysaccharide vaccine does not significantly reduce the rates of fatal or nonfatal acute coronary syndrome and ischemic stroke over approximately seven years in adults aged 55 to 60 years with multiple cardiovascular risk factors but no prior cardiovascular events. The study was limited by a lower than expected number of events, resulting in reduced power.
These findings provide important evidence against a cardiovascular protective role of PPV23 in this population, indicating that pneumococcal vaccination should remain centered on infection prevention according to current clinical guidelines rather than cardiovascular risk modification.
Future research may explore whether other vaccine types or populations might achieve cardiovascular benefits.
References
1. Hure A, Peel R, D’Este C, et al. Prevention of Adverse Cardiovascular Events Using the 23-Valent Pneumococcal Polysaccharide Vaccine: A Randomized Clinical Trial. JAMA Cardiol. 2025 Sep 17:e253043. doi:10.1001/jamacardio.2025.3043. Epub ahead of print. PMID: 40960793; PMCID: PMC12444640.
2. Ridker PM. Inflammation, atherosclerosis, and cardiovascular risk: an epidemiologic view. Blood Coagul Fibrinolysis. 1997;8 Suppl 1:S13-9.
3. Grondman I, Ottenhoff TH, Netea MG. Innate immune memory: implications for host responses to infection and vaccination. Clin Microbiol Infect. 2019;25(3):261-266. doi:10.1016/j.cmi.2018.11.015.
4. Lancellotti P, et al. The Role of Inflammation in Cardiovascular Disease: Current Understanding and Future Perspectives. Eur J Intern Med. 2023;108:54-63.