Highlights
Validated Diagnostic Threshold
The study identifies a summative score of >12/60 on pelvic muscle palpation as a highly accurate threshold (sensitivity 82.3%; specificity 79.1%) for diagnosing high tone pelvic floor dysfunction (HTPFD).
Distinct Clinical Phenotype
Patients meeting the HTPFD threshold are significantly more likely to experience persistent pain (at least 14 days per month) and report systemic symptoms like nausea and vomiting.
Activity-Induced Exacerbation
HTPFD is strongly associated with pain triggered by physical activities, specifically exercise and walking, distinguishing it from other pelvic pain etiologies.
Severe Sexual Dysfunction
Dyspareunia, including pain persisting for 24 hours post-intercourse and the avoidance of sexual activity, remains a hallmark clinical feature of HTPFD.
Background: The Challenge of Pelvic Myofascial Pain
Chronic pelvic pain (CPP) affects approximately 15% to 25% of women worldwide, yet its diagnosis remains one of the most complex challenges in gynecology and urology. Among the various contributors to CPP, high tone pelvic floor dysfunction (HTPFD)—characterized by overactive, non-relaxing pelvic floor muscles—is increasingly recognized as a primary driver of symptoms. Despite this recognition, the clinical landscape has long been hampered by a lack of standardized diagnostic criteria. Traditionally, the identification of HTPFD has relied heavily on expert opinion and subjective clinical assessment rather than reproducible, data-driven thresholds. This lack of consensus creates significant barriers to clinical identification, hinders the evaluation of treatment efficacy (such as pelvic floor physical therapy or Botox injections), and delays necessary care for patients. The study by Till et al. (2025) addresses this gap by establishing a quantitative myofascial tenderness score that correlates with patient-reported pain reproduction.
Study Design and Methodology
This cross-sectional study analyzed data from 612 patients who presented to a specialized chronic pelvic pain referral center between July 2019 and January 2023. The methodology focused on bridging the gap between physical examination findings and patient-reported symptoms.
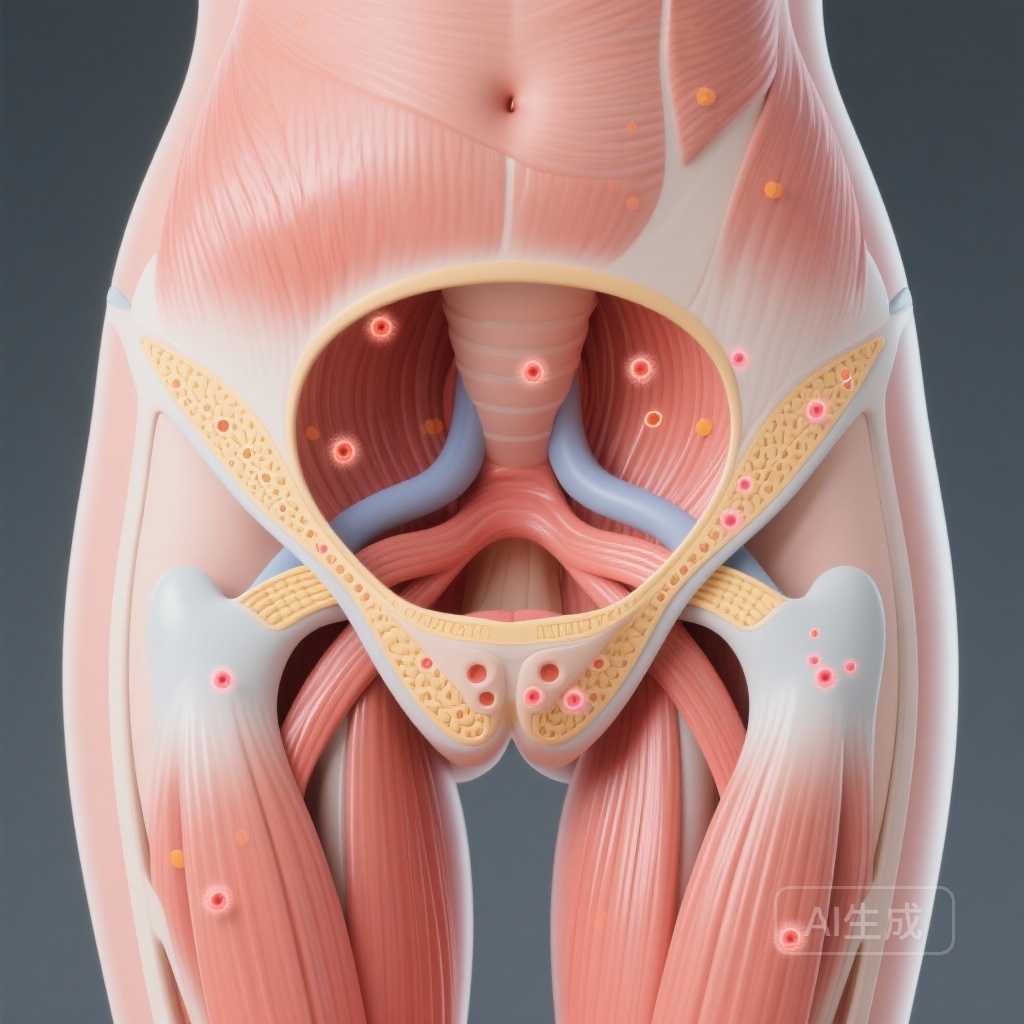
Standardized Physical Examination
Prior to their first visit, patients completed comprehensive questionnaires regarding pain frequency, intensity, and impact on daily life. During the initial clinical encounter, a standardized physical examination was performed. This involved the palpation of six specific pelvic muscle sites: the bilateral pubococcygeus, iliococcygeus, and obturator internus. Each site was assessed using a numerical scale, resulting in a summative tenderness score out of a possible 60.
Statistical Analysis
The researchers utilized Receiver Operating Characteristic (ROC) curve analyses to determine the optimal summative tenderness score that corresponded to the reproduction of the patient’s primary pain complaint. Comparative analyses were then conducted to evaluate the clinical differences between patients who met this diagnostic threshold and those who did not.
Key Findings: Establishing the >12/60 Threshold
The study’s primary achievement is the identification of a diagnostic cutoff that balances sensitivity and specificity. A summative score of >12/60 on palpation demonstrated a sensitivity of 82.3% and a specificity of 79.1%. This threshold proved superior to previously utilized, less rigorous classification methods.
Prevalence and Pain Characteristics
Using this >12/60 threshold, 63.6% (n=389) of the cohort were categorized as having HTPFD. These patients exhibited a more severe and persistent clinical profile compared to the non-HTPFD group:
Frequency and Quality of Pain
Patients with HTPFD were significantly more likely to experience persistent pain, defined as at least 14 pain days per month (Odds Ratio [OR] 2.32, 95% CI 1.60–3.35, p<.001). Furthermore, they often described their pain as a heavy feeling in the pelvis and reported pain radiation to other body regions.
Activity and Systemic Impact
A defining characteristic of HTPFD identified in this study is the exacerbation of pain through physical movement. Patients were more likely to report pain during exercise (OR 1.69) and walking (OR 1.85). Additionally, the HTPFD group reported a higher incidence of systemic symptoms, including nausea and vomiting (p<.001), suggesting a potential overlap with central sensitization or high autonomic arousal.
The Impact on Sexual Health
Sexual dysfunction emerged as a critical and highly significant symptom of HTPFD. The study found that patients with HTPFD reported significantly worse sexual function across multiple metrics. They experienced more severe and consistent dyspareunia, with pain not only occurring during intercourse but often continuing for up to 24 hours afterward. This persistent post-coital pain led to a significantly higher rate of interrupting or entirely avoiding intercourse compared to patients without HTPFD (all p<.001). These findings suggest that HTPFD is not merely a localized muscle issue but a condition that profoundly impacts intimacy and quality of life.
Expert Commentary: Mechanistic Insights and Clinical Utility
The establishment of a 12/60 tenderness score represents a major step toward the objective quantification of pelvic floor disorders. From a mechanistic perspective, the association between HTPFD and pain exacerbation during walking or exercise is biologically plausible; the pelvic floor muscles act as a core stabilizer during gait and physical activity. When these muscles are already hypertonic or in a state of constant contraction, the additional demand of physical activity likely leads to rapid fatigue and nociceptive signaling.
Clinical Generalizability
While the study provides a robust data-driven threshold, clinicians should consider the context of a referral center population, which may represent more complex cases. However, the use of a standardized 0-10 scale for specific muscle groups provides a template that can be easily integrated into general gynecological practice. This move away from binary (presence/absence) assessments to a summative score allows for more nuanced tracking of patient progress over time, particularly during interventions like pelvic floor physical therapy.
Study Limitations
As a cross-sectional study, these findings show association rather than causation. Further longitudinal research is required to determine if reducing the tenderness score through treatment directly correlates with the resolution of symptoms like dyspareunia or activity-induced pain.
Conclusion: A New Standard for Pelvic Health
High tone pelvic floor dysfunction should be a primary consideration for any patient presenting with a summative tenderness score of >12/60 across the pubococcygeus, iliococcygeus, and obturator internus. The study confirms that HTPFD is associated with a distinct clinical phenotype characterized by persistent, radiating pain, activity-induced flares, and severe sexual dysfunction. By adopting these standardized diagnostic criteria, clinicians can better identify HTPFD, tailor treatment strategies more effectively, and ultimately improve outcomes for women living with chronic pelvic pain.
References
Till SR, Schrepf A, Arewasikporn A, Kratz AL, Missmer SA, As-Sanie S. Data-driven diagnosis and clinical presentation of high tone pelvic floor dysfunction. Am J Obstet Gynecol. 2025 Dec 17:S0002-9378(25)00933-0. doi: 10.1016/j.ajog.2025.12.036. Epub ahead of print. PMID: 41419153.