Highlight
Pediatric acute care in the US is regionally distinct and existing adult-based geographic frameworks inadequately capture pediatric use patterns. This landmark study employed Medicaid data from over 27 million encounters to develop the first empirically derived pediatric-specific Acute Care Atlas comprising Pediatric Emergency Service Areas (PESAs) and Pediatric Emergency Referral Regions (PERRs). The new atlas demonstrated higher modularity and retention of patient encounters within regions compared to existing adult or mixed-population atlases, underscoring the value of pediatric-specific mapping for research, policy, and healthcare quality improvement.
Study Background
Healthcare regionalization—the organization of acute care services within defined geographic boundaries—facilitates coordinated patient care, efficient resource allocation, and quality improvement. While regionalization frameworks for acute care exist based largely on adult care patterns, they inadequately represent pediatric needs due to significant differences in healthcare utilization, referral pathways, and hospital capabilities for children. Pediatric emergency care is highly regionalized, with unique network structures shaped by children’s hospitals and pediatric specialty centers. Yet, a national-standardized pediatric acute care mapping system has been lacking. Addressing this unmet need is critical to optimize healthcare delivery, conduct relevant outcomes research, and inform pediatric health policy across the United States.
Study Design
This cross-sectional study analyzed Medicaid and Children’s Health Insurance Program (CHIP) data from January 2021 through December 2022, encompassing emergency and inpatient pediatric encounters among youth under 16 years of age, who represent over 50% of US children. Data were derived from 4830 acute care hospitals nationwide. The study employed advanced network analysis methodologies to develop pediatric-specific geographic units: Pediatric Emergency Service Areas (PESAs), which encapsulate home-to-hospital care-seeking behaviors, and Pediatric Emergency Referral Regions (PERRs), which reflect interhospital referral patterns. The study compared these new units to existing adult-centric geography frameworks, including Dartmouth Atlas Hospital Service Areas (HSAs), pediatric HSAs (PHSAs), Hospital Referral Regions (HRRs), pediatric HRRs (PHRRs), and state boundaries. Key outcomes included measures of modularity, which quantify how well these geographic groupings capture patient flow patterns, along with size metrics, hospital counts, and internal encounter retention percentages.
Key Findings
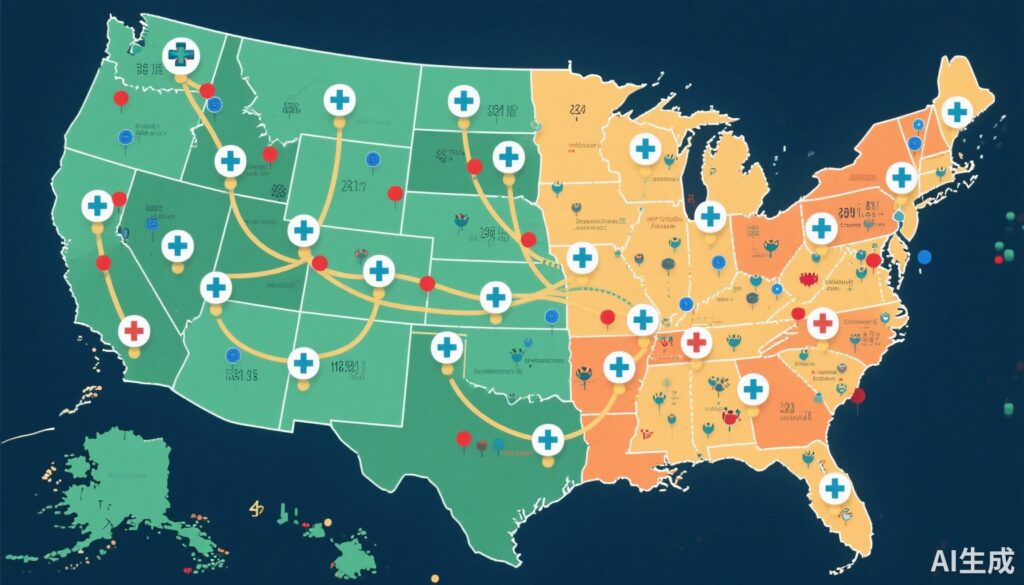
From 27,817,736 acute care encounters collected, the analysis identified 835 PESAs and 105 PERRs across the US pediatric population. Compared to adult-based HSAs and PHSAs, PESAs were larger both in geographic area and population covered, incorporating more hospitals and children. Specifically, PERRs were substantially larger than HRRs or PHRRs, covering median areas of 17,595 square miles versus 4,822 and 8,845 square miles respectively, and included more hospitals (median of 39 vs. 11 and 21) and youths (median 597,000 vs. 146,000 and 348,000).
Regarding modularity, PESAs exhibited superior local-level modularity, indicating a greater concordance with where patients sought initial acute care. PERRs showed the highest referral-level modularity, accurately representing interhospital transfer patterns and referral networks. Observed encounter retention was highest within PESAs (89.9%) compared to HSAs (68.6%) and PHSAs (80.1%). Similarly, 92.3% of referrals remained within PERRs, outperforming HRRs (73.0%), PHRRs (81.9%), and closely approximating state-level retention (93.4%).
The newly constructed atlas thus demonstrated enhanced fidelity to real-world pediatric care-seeking and referral behaviors, emphasizing the limitations of adult-derived regionalization models in capturing pediatric healthcare dynamics.
Expert Commentary
The development of a pediatric-specific Acute Care Atlas represents a pivotal advancement in health services research and pediatric care planning. By grounding the atlas in empirical Medicaid and CHIP encounter data, the authors created a realistic map that reflects pediatric utilization patterns rather than extrapolations from adult data. Such specificity is vital given the concentration of pediatric expertise in specialized hospitals and the existence of unique referral streams distinct from adult networks.
These findings suggest significant implications for research and policy. For instance, this atlas offers a nuanced framework to study regional pediatric healthcare quality, outcomes disparities, and resource allocation. Moreover, states and healthcare systems may leverage this mapping to optimize emergency care infrastructure, streamline referrals, and implement quality improvement initiatives targeted for children.
Limitations include the reliance on Medicaid and CHIP populations, which although representing a majority of US children, may underrepresent privately insured cohorts and hence certain geographic or socioeconomic variations. Additionally, the atlas focuses on acute emergency and inpatient encounters, with future work needed to integrate outpatient and subspecialty pediatric care networks.
Conclusion
The Atlas of Pediatric Acute Care stands as the first empirically derived, pediatric-focused national map of acute care regions in the United States. By accurately modeling pediatric patient flows and referral networks, this atlas provides a foundational tool for future pediatric clinical research, health policy-making, regional planning, and quality improvement efforts. Adoption of this atlas can address long-standing gaps in pediatric healthcare regionalization and ultimately enhance health outcomes for children nationally.
Funding and ClinicalTrials.gov
No specific funding or clinical trial registration was reported for this study.
References
- Michelson KA, Skol AD, Graves JA, Remick KE, McMullen PD, Singamsetty N, Cory DK, Bucholz EM. Development of an Atlas for US Pediatric Acute Care. JAMA Pediatr. 2025 Oct 27. doi: 10.1001/jamapediatrics.2025.4227. Epub ahead of print. PMID: 41143815.