Study Background and Disease Burden
Heart failure with preserved ejection fraction (HFpEF) is a complex clinical syndrome characterized by impaired cardiac relaxation and elevated filling pressures despite normal left ventricular ejection fraction. It accounts for approximately half of all heart failure cases and remains challenging to treat effectively. Obesity is a major contributing factor to HFpEF pathogenesis and progression, often associated with systemic inflammation, increased volume overload, and comorbidities.
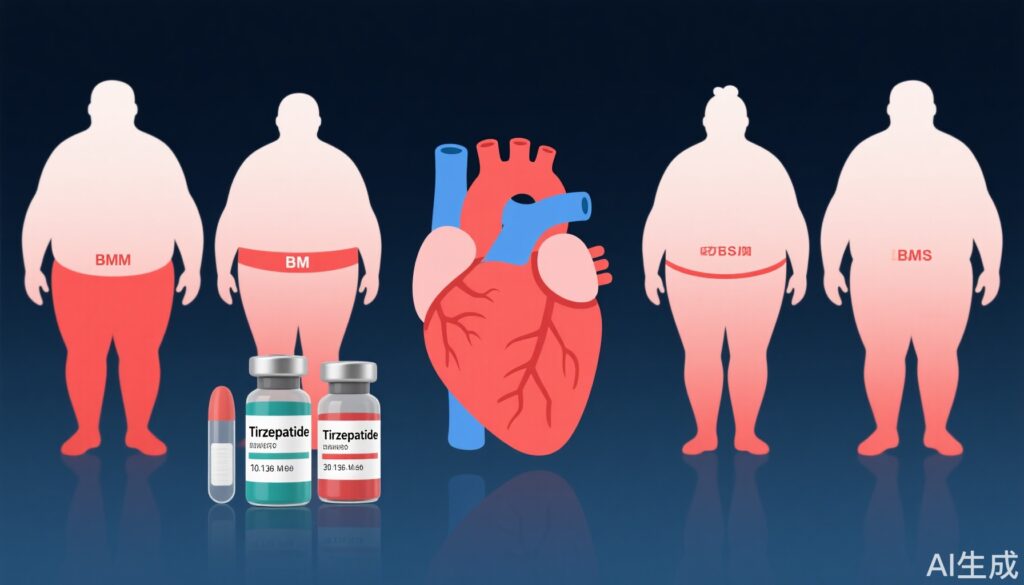
The SUMMIT trial investigated tirzepatide, a novel dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, for its cardiovascular benefits in patients with obesity-related HFpEF. Tirzepatide has previously demonstrated robust effects on glycemic control and weight reduction in diabetes and obesity populations. Given the heterogeneity in obesity phenotypes, notably differences in body mass index (BMI) and central adiposity measured via waist-height ratio (WHR), understanding how these factors modulate tirzepatide’s efficacy in HFpEF is critical.
Study Design
The SUMMIT trial was a randomized, placebo-controlled study including 731 patients with New York Heart Association (NYHA) functional class II-IV HFpEF and BMI ≥30 kg/m2. Patients were randomly assigned to receive tirzepatide (n = 364) or placebo (n = 367) and followed for 52 weeks.
Primary endpoints were time to cardiovascular death or worsening heart failure and change from baseline in Kansas City Cardiomyopathy Questionnaire Clinical Summary Score (KCCQ-CSS) at 52 weeks. Secondary outcomes included changes in 6-minute walk distance (6MWD), C-reactive protein (CRP) levels, and body weight (BW).
In this secondary analysis, outcomes were stratified by baseline obesity severity according to BMI tertiles and obesity distribution according to WHR tertiles. Cox regression models assessed time-to-event outcomes, while mixed-effects models for repeated measures analyzed continuous variables. Relationships between changes in BW and waist circumference (WC) and clinical endpoints were also explored within the tirzepatide group.
Key Findings
Patients with higher baseline BMI were generally younger, more often female, and exhibited more severe heart failure symptoms and physical limitations. Notably, this group showed greater volume overload despite higher diuretic use, lower natriuretic peptide levels, and elevated systemic inflammation compared to those with lower BMI. Similar observations were found when stratifying by WHR; however, patients with elevated WHR faced more pronounced kidney dysfunction and reduced exercise capacity.
Tirzepatide significantly reduced the risk of cardiovascular death or worsening heart failure compared to placebo across all BMI and WHR tertiles, with no heterogeneity in treatment effect noted by obesity severity or fat distribution.
Importantly, higher BMI tertiles corresponded with greater improvements in 6MWD (estimated treatment difference [ETD]: 9.9 m in lowest vs 37.5 m in highest BMI tertile; P=0.025), larger reductions in body weight (-10.7% to -14.4%; P=0.006), and systolic blood pressure (-1.00 to -6.65 mm Hg; P=0.035). A trend toward greater enhancement of KCCQ-CSS was also observed with increasing BMI (P=0.097).
Within the tirzepatide-treated cohort, weight loss magnitude strongly correlated with improvements in key clinical parameters: patients who lost more weight experienced greater gains in 6MWD, enhanced KCCQ-CSS, reduced CRP levels, and lowered blood pressure. Similarly, greater decreases in WC were associated with improved exercise capacity and symptom scores, emphasizing the clinical relevance of targeting central adiposity.
Individuals with elevated WHR but lower BMI demonstrated more advanced heart failure (higher NYHA class), elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP), worse renal function, and reduced exercise capacity relative to those with lower WHR and higher BMI, underscoring the distinct risk profiles conferred by fat distribution independent of overall obesity.
Expert Commentary
The SUMMIT trial extends our understanding of tirzepatide’s therapeutic potential in obesity-related HFpEF by integrating insights into obesity phenotypes. The consistent cardiovascular risk reduction regardless of BMI or central adiposity suggests tirzepatide’s benefits surpass metabolic improvements alone, possibly related to anti-inflammatory and hemodynamic effects. The observed dose-response relationship between weight loss and clinical benefit underlines the importance of weight reduction as a treatment target in HFpEF.
The greater improvements in 6MWD among higher BMI patients may reflect a greater baseline functional reserve or more reversible physiological impairment. Meanwhile, elevated WHR identifying patients with poorer renal function and exercise tolerance highlights the need for tailored management strategies addressing central obesity and its sequelae.
Limitations include the secondary nature of this analysis and the potential influence of confounding factors inherent in observational comparisons within trial data. Further studies are needed to elucidate mechanistic pathways linking adiposity distribution and treatment responses.
Conclusion
In patients with obesity-related HFpEF, tirzepatide reliably reduces the incidence of cardiovascular death or worsening heart failure across varying degrees of obesity severity and central adiposity. Greater BMI and associated weight loss correlate with enhanced improvements in functional capacity and symptom burden. Monitoring and targeting central adiposity may further refine risk stratification and therapeutic outcomes.
These findings support tirzepatide as a promising intervention that addresses both metabolic and cardiovascular aspects of HFpEF in obesity, marking a significant advance in managing this multifaceted syndrome. Ongoing research should focus on optimizing individualized treatment approaches based on comprehensive obesity phenotyping.
References
Borlaug BA, Zile MR, Kramer CM, Ye W, Ou Y, Hurt K, Murakami M, Packer M; SUMMIT Trial Study Group. Impact of Body Mass Index, Central Adiposity, and Weight Loss on the Benefits of Tirzepatide in HFpEF: The SUMMIT Trial. J Am Coll Cardiol. 2025 Jul 29;86(4):242-255. doi: 10.1016/j.jacc.2025.04.059. PMID: 40701669.