Highlight
- Time-restricted eating (TRE) significantly reduces hepatic steatosis in patients with metabolic dysfunction-associated steatotic liver disease (MASLD) over 16 weeks.
- TRE shows similar efficacy to traditional calorie restriction (CR) regarding weight loss, body composition, and metabolic parameters.
- No serious adverse events were reported, suggesting TRE is a safe and practical dietary strategy for MASLD management.
Study Background
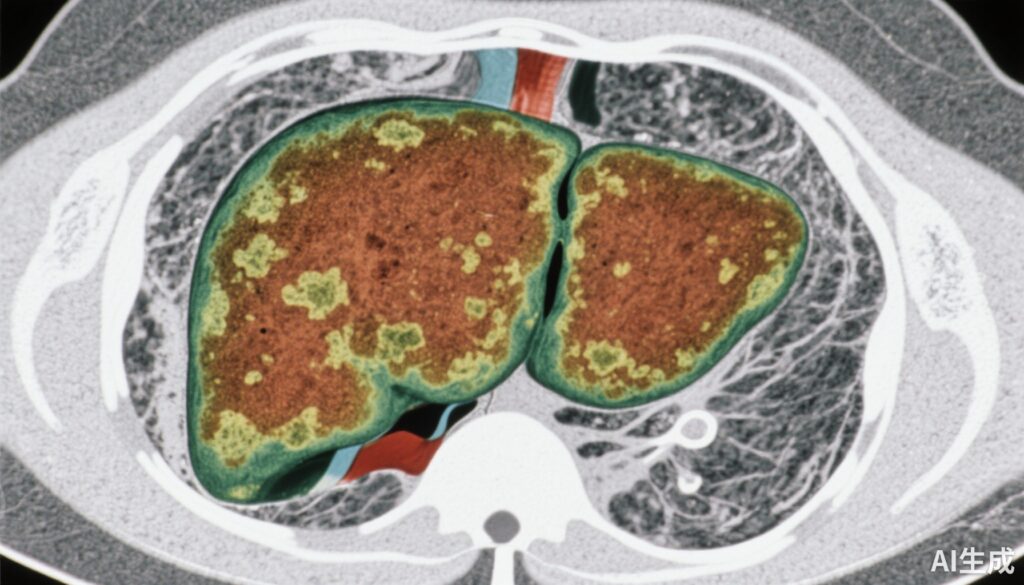
Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as nonalcoholic fatty liver disease (NAFLD), represents a growing public health concern worldwide, paralleling the rise in obesity and metabolic syndrome. Characterized by excessive hepatic fat accumulation and often accompanied by insulin resistance and systemic inflammation, MASLD predisposes affected individuals to progressive liver fibrosis, cirrhosis, and cardiovascular morbidity. Lifestyle interventions remain the cornerstone of MASLD management, with weight loss proven to mitigate hepatic steatosis and improve metabolic health.
Traditional calorie restriction (CR) has demonstrated efficacy in reducing liver fat and improving associated metabolic parameters. However, adherence to long-term caloric limitation can be challenging. Time-restricted eating (TRE), a form of intermittent fasting restricting food intake to defined daily windows without prescribed caloric reduction, has recently gained attention as a potentially sustainable lifestyle modification capable of improving weight management, insulin sensitivity, and body composition.
Despite promising metabolic benefits of TRE observed in other populations, evidence regarding its effectiveness and safety specifically in patients with MASLD is limited. This randomized controlled trial aimed to clarify whether TRE could serve as an effective dietary intervention for patients with overweight or obesity and established MASLD, compared to standard of care and conventional calorie restriction.
Study Design
This was a 16-week, single-center, randomized controlled trial enrolling 337 adult patients diagnosed with MASLD who were overweight or obese. Participants were randomized in a 1:1:1 ratio into three intervention arms:
- Standard of Care (SOC): Received general lifestyle advice without any specific dietary modification protocol.
- Calorie Restriction (CR): Prescribed a hypocaloric diet aimed at reducing daily caloric intake to achieve weight loss.
- Time-Restricted Eating (TRE): Instructed to restrict their daily food intake to a specific time window each day (e.g., 8–10 hours), without explicit caloric limitation.
The primary outcome was improvement in hepatic steatosis measured quantitatively by MRI-based proton density fat fraction (MRI-PDFF). Secondary endpoints included changes in liver stiffness (reflecting fibrosis), body composition (weight, waist circumference, fat mass), lipid profiles, glucose homeostasis, and sleep quality. Safety and adverse events were systematically monitored throughout.
Key Findings
A total of 333 participants completed the study per full analysis set (113 SOC, 110 CR, 110 TRE). Baseline characteristics were balanced across groups. After 16 weeks, the TRE group exhibited a significant reduction in hepatic steatosis, with MRI-PDFF decreasing by 25.8%, whereas the SOC group showed minimal change (0.7%). The CR group had a nearly identical reduction to TRE (24.7%), confirming comparable efficacy.
Regarding body composition, the TRE group achieved meaningful decreases in body weight, waist circumference, and fat mass, surpassing SOC but similar to CR. These anthropometric improvements coincided with favorable trends in metabolic parameters including glucose homeostasis and lipid profiles, although differences between TRE and CR were not statistically significant.
Liver stiffness measurements did not differ substantially between TRE and CR, indicating no significant impact on fibrosis over this short duration. Sleep quality assessments were also comparable between TRE and CR groups.
Importantly, the TRE intervention was well tolerated, with no serious adverse events reported, supporting its safety in this patient population.
Expert Commentary
This randomized trial provides robust evidence supporting the utility of TRE as a non-pharmacologic intervention for MASLD. The magnitude of hepatic fat reduction parallels that achieved by traditional caloric restriction, suggesting that modifying meal timing alone may efficiently modulate hepatic lipid metabolism and insulin sensitivity.
Mechanistically, TRE may exert benefits by restoring circadian rhythm alignment and enhancing metabolic flexibility of hepatocytes, which could reduce lipogenesis and promote lipid oxidation. While the 16-week duration limits conclusions regarding long-term effects on fibrosis progression, these findings are clinically relevant given the current paucity of approved MASLD therapies and the challenges in maintaining caloric restriction.
Notably, the trial’s single-center design and lack of participant blinding may predispose to biases. Additionally, adherence to prescribed eating windows and dietary patterns outside timing control were not extensively discussed, factors critical in real-world application. Future multicenter trials with extended follow-up and mechanistic biomarkers will help delineate the broader applicability of TRE in MASLD.
Conclusion
Time-restricted eating is an effective and safe dietary approach that significantly reduces hepatic steatosis in patients with MASLD, delivering metabolic benefits comparable to calorie restriction. Its practical nature and tolerability may enhance adherence compared to strict caloric reduction, positioning TRE as a promising strategy for MASLD management. These encouraging results warrant further long-term investigations to establish sustained efficacy, impact on fibrosis, and integration into comprehensive care protocols.
Funding and ClinicalTrials.gov
The trial was registered at ClinicalTrials.gov (NCT05579158). Funding sources were not specified in the provided summary.
References
Oh JH, Yoon EL, Park H, Lee S, Jo AJ, Cho S, Kwon E, Nah EH, Lee JH, Park JH, Ahn SB, Jun DW. Efficacy and safety of time-restricted eating in metabolic dysfunction-associated steatotic liver disease. J Hepatol. 2025 Jun 19:S0168-8278(25)02272-X. doi: 10.1016/j.jhep.2025.06.005. Epub ahead of print. PMID: 40543603.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328-357.
Longo VD, Panda S. Fasting, circadian rhythms, and time-restricted feeding in healthy lifespan. Cell Metab. 2016;23(6):1048-1059.