Study Background and Disease Burden
Chronic Obstructive Pulmonary Disease (COPD) remains a leading cause of morbidity and mortality worldwide, particularly in its very severe stages. Patients afflicted with advanced COPD often suffer profound breathlessness and marked exercise intolerance, largely due to expiratory flow limitation and impaired ventilatory mechanics. These physiological derangements not only reduce quality of life but also complicate management strategies, especially for those awaiting lung transplantation. Pulmonary rehabilitation, including exercise training combined with respiratory support such as non-invasive ventilation (NIV) or high-flow nasal therapy (HFT), aims to ameliorate symptoms and enhance functional capacity. However, heterogeneity in patient responses highlights the need for better predictive tools and individualized treatment approaches.
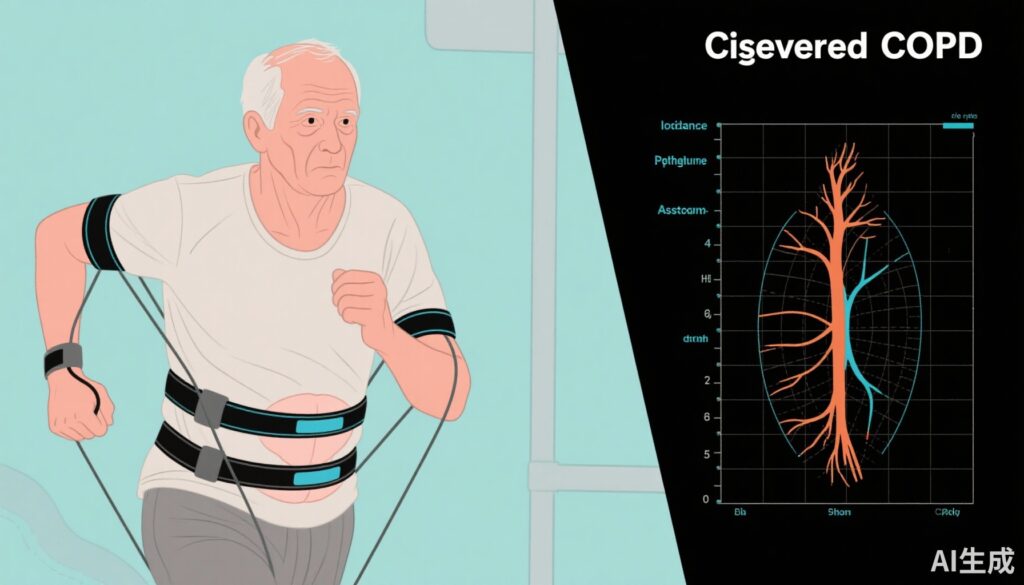
Respiratory mechanics in COPD are inherently complex; thoracoabdominal asynchrony (TAA) — a dis-coordination between chest wall and abdominal movements during breathing — emerges as an important physiological marker. Understanding how TAA relates to lung function impairment, dyspnoea severity during exercise, and responses to respiratory support may refine rehabilitation and management of severe COPD.
Study Design
The study by Sayas Catalán et al. was an experimental, longitudinal, prospective, controlled analysis involving 20 patients with very severe COPD enlisted for lung transplantation. Each participant underwent three constant load exercise tests under three different respiratory support conditions: conventional oxygen therapy (COT, unsupported), non-invasive ventilation (NIV), and high-flow nasal therapy (HFT).
TAA was quantitatively assessed using respiratory inductance plethysmography, a non-invasive method measuring changes in thoracic and abdominal circumference during breathing cycles, capable of detecting timing and amplitude differences between compartments. Neurorrespiratory drive (NRD), an electrophysiological measure of the central respiratory motor output to the parasternal intercostal muscles, was concurrently measured by parasternal electromyography, providing insights into respiratory neural activation under different exercise and support scenarios. Key clinical parameters, including baseline lung function tests and Borg dyspnoea scores at peak exercise, were recorded.
Key Findings
Distinct patterns of TAA emerged during exercise among the studied cohort. Patients manifested either clockwise rotation (thorax moving ahead of the abdomen) or counterclockwise (abdomen leading the thorax). Importantly, clockwise rotation was significantly associated with poorer baseline lung function metrics, including more severe expiratory airflow obstruction and reduced lung volumes. Additionally, these patients experienced greater peak exercise dyspnoea and elevated peak NRD, indicative of higher respiratory muscle workload and neural drive.
Comparative analysis of exercise under COT, NIV, and HFT conditions revealed that TAA patterns remained stable across these modalities; no significant shifts in asynchrony direction or magnitude were detected. Notably though, patients exhibiting clockwise rotation were more likely to demonstrate clinically meaningful reductions in breathlessness when exercised with NIV compared to COT. Contrastingly, those with counterclockwise TAA showed less predictable improvements with respiratory support.
These findings suggest that TAA direction during exercise serves as a physiological marker of disease severity and may predict individual responsiveness to certain modalities of non-invasive respiratory support. Although HFT was evaluated, its impact regarding TAA and symptomatic relief seemed less pronounced than NIV in this population.
Expert Commentary
The results presented by Sayas Catalán et al. offer valuable mechanistic insights into the interplay between respiratory mechanics, neural respiratory drive, and symptomatic limitations in very severe COPD. Measuring TAA provides an integrative assessment of ventilatory dynamics, beyond traditional spirometry. The identified correlation between clockwise TAA and worse lung function aligns with the pathophysiological understanding that asynchronous chest wall motion reflects mechanical constraints imposed by lung hyperinflation and diaphragmatic dysfunction.
The ability of NIV to alleviate breathlessness preferentially in patients with clockwise TAA may relate to its capacity to unload respiratory muscles and improve ventilatory synchrony. This raises the prospect of utilizing TAA and NRD monitoring as biomarkers to personalize rehabilitation interventions, selecting patients who may derive the greatest benefit from supported ventilation during exercise.
Nonetheless, the study’s sample size limits broad generalizability, and the stable TAA patterns across support modes prompt further inquiry into whether alternative or adjunctive interventions can modulate thoracoabdominal coordination. Moreover, longitudinal assessments during rehabilitation programs would clarify if TAA changes track clinical improvement.
Conclusion
Thoracoabdominal asynchrony during exercise emerges as a novel physiological and clinical indicator in very severe COPD, reflecting underlying pulmonary impairment and exertional dyspnoea severity. The differentiation of TAA patterns—particularly clockwise rotation—can help stratify patients according to disease severity and potentially predict responsiveness to non-invasive ventilation during rehabilitation. This approach paves the way for more individualized management strategies enhancing quality of life in this challenging population.
Future research should focus on validating TAA and NRD measurements in larger cohorts and exploring their integration into comprehensive pulmonary rehabilitation protocols to optimize respiratory support and functional outcomes in severe COPD.
References
Sayas Catalán J, Lalmolda C, Hernández-Voth A, Corral Blanco M, Murphy P, Gonzalez-Ramos L, Florez-Solarana P, Lloret-Puig B, Lujan M. Thoracoabdominal Asynchrony in Very Severe COPD: Clinical and Functional Correlates During Exercise. Arch Bronconeumol. 2025 Sep;61(9):544-554. doi: 10.1016/j.arbres.2025.01.010. Epub 2025 Jan 31. PMID: 39952874.
Additional sources:
Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2024 Report. Global Strategy for Prevention, Diagnosis and Management of COPD.
AI Image Prompt: “Illustration of a severe COPD patient performing exercise with respiratory inductance plethysmography bands showing thoracoabdominal asynchrony, alongside graphical depiction of neurorrespiratory drive monitoring.”