Highlights
– A 12-week therapist-guided internet-based cognitive behavioral therapy (ICBT) program tailored to Japanese culture significantly reduced weekly combined frequency of binge eating and compensatory behaviors compared with usual care (adjusted mean difference 9.84 episodes; 95% CI, 2.49–17.18; P = .01; Cohen d = 0.73).
– Trial enrolled 61 women with DSM-5 bulimia nervosa across seven university hospitals in Japan; primary endpoint assessed by blinded independent raters at 12 weeks.
– Findings support ICBT as an accessible, clinically effective adjunct to usual care for women with bulimia nervosa in East Asian clinical settings, though generalizability beyond the trial population and long-term durability require further study.
Study background and disease burden
Bulimia nervosa is a serious eating disorder characterized by recurrent binge eating episodes followed by compensatory behaviors such as self-induced vomiting, laxative misuse, fasting, or excessive exercise. The disorder carries substantial psychiatric morbidity (including high rates of depression, anxiety, and suicidality), medical complications (electrolyte disturbances, gastrointestinal injury, dental erosion), and functional impairment. Although cognitive behavioral therapy (CBT) is established as an evidence-based first-line psychological treatment for bulimia nervosa, many patients lack timely access to specialist CBT because of workforce shortages, stigma, geographic barriers, and cost.
Internet-delivered CBT (ICBT) with therapist guidance has been explored in several mental health conditions as a way to increase scalability while preserving therapist support. However, evidence for ICBT specifically for bulimia nervosa in clinical settings in East Asia has been limited. The trial led by Hamatani et al. (JAMA Network Open, 2025) evaluated a culturally adapted, guided ICBT program for women with bulimia nervosa in Japan to address this gap.
Study design
This investigator-initiated randomized clinical trial enrolled female outpatients aged 13–65 years meeting DSM-5 criteria for bulimia nervosa, with BMI ≥ 17.5, internet access, and no CBT-related treatment within the prior 2 years. Recruitment and treatment occurred at seven university hospitals in Japan between August 2022 and October 2024. Participants (n = 61) were randomized to usual care alone (control, n = 30) or usual care plus therapist-guided ICBT (intervention, n = 31).
The intervention consisted of a 12-week ICBT program grounded in a specified cognitive behavioral model and adapted for Japanese cultural context. Program content included modules addressing regular eating scheduling, cognitive restructuring, behavioral experiments, exposure to avoided foods or situations, relapse prevention, and self-monitoring. Therapists provided asynchronous and/or scheduled guidance to support module completion, problem solving, and therapeutic alliance. Both groups continued to receive usual care from their treating clinicians, which could include pharmacotherapy, medical monitoring, or non-CBT psychosocial support.
The prespecified primary outcome was the weekly combined frequency of binge eating and compensatory behaviors measured at baseline and at 12 weeks by a blinded, independent rating team. Intention-to-treat (ITT) analyses used linear mixed models; effect sizes were reported as Cohen d. The trial was registered in the UMIN Clinical Trials Registry (UMIN00048732).
Key findings
Population characteristics
– N = 61 randomized: 31 to ICBT + usual care, 30 to usual care alone.
– Mean (SD) age 27.8 (9.0) years; mean (SD) BMI 21.1 (3.6); mean (SD) illness duration 9.3 (8.8) years.
– Approximately half (50.8%) were employed.
Primary outcome
– Intent-to-treat analysis demonstrated a statistically and clinically meaningful reduction in weekly combined frequency of binge and compensatory episodes in the guided ICBT group versus control at 12 weeks.
– Adjusted mean difference: 9.84 fewer episodes per week (95% CI, 2.49–17.18 episodes); P = .01.
– Effect size: Cohen d = 0.73 (95% CI, 0.21–1.26), consistent with a moderate-to-large effect.
– Sensitivity analyses (not detailed here) reportedly supported robustness of the primary result.
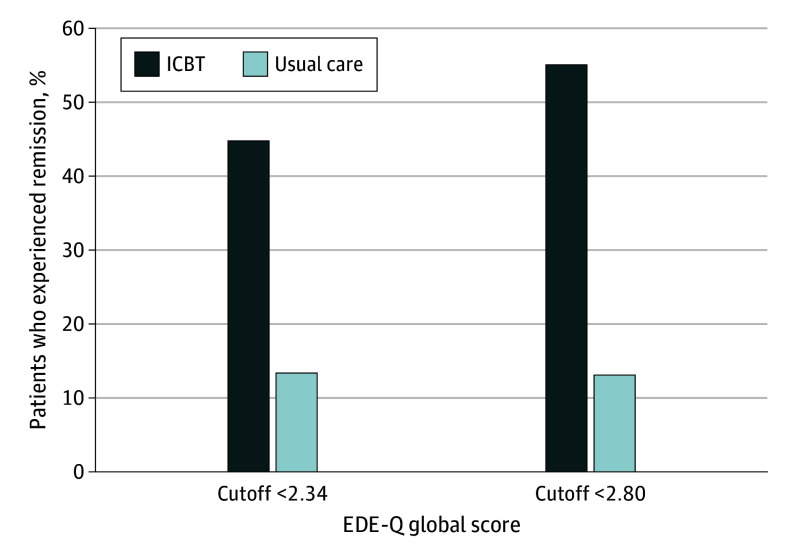
Participants in Remission in Each Group.
Secondary and acceptability outcomes
– The report emphasizes the acceptability of the therapist-guided ICBT program to participants; while precise adherence and dropout metrics are not reproduced here, the authors concluded that acceptability was adequate to support clinical deployment.
Safety and adverse events
– The published abstract and main text highlight effectiveness and acceptability; they do not report unexpected safety signals. Standard clinical monitoring was part of usual care. The study excluded individuals with BMI < 17.5, thereby reducing the immediate risk of severe anorexia-related medical complications in the trial cohort.
Interpretation of effect size and clinical relevance
– A reduction of nearly 10 combined episodes per week is clinically meaningful for patients with bulimia nervosa, given the high baseline frequency commonly reported in clinical samples.
– Cohen d of 0.73 indicates a moderate-to-large effect compared with usual care over a 12-week timeframe, comparable with or favorable to many brief psychological interventions in this population.
Expert commentary and contextualization
Clinical context
– Cognitive behavioral therapy remains the recommended first-line psychological treatment for bulimia nervosa; however, access barriers are substantial. Therapist-guided ICBT aims to retain core CBT procedures while increasing reach through remote delivery, asynchronous content, and efficient therapist time use.
Strengths of the trial
– Randomized, multicenter design across seven university hospitals increases internal validity and reduces center-specific bias.
– Primary outcome assessed by blinded independent raters reduces detection bias.
– Cultural adaptation of content to Japanese patients addresses acceptability and relevance, an important consideration for psychotherapy dissemination.
Limitations and considerations
– Sample size (n = 61) is modest; although the effect reached statistical significance, replication in larger and diverse samples would increase confidence in generalizability.
– Female-only enrollment limits inference to men and nonbinary patients with bulimia nervosa.
– Short-term endpoint (12 weeks) documents early efficacy; maintenance of gains beyond the treatment window (e.g., 6–12 months) was not reported here and is crucial for long-term outcomes and relapse prevention.
– Usual care as the comparator is pragmatic but heterogeneous; active comparators (face-to-face CBT, guided self-help, or attention-matched controls) would better isolate the incremental value of ICBT format and therapist guidance.
– Exclusion of patients with BMI < 17.5 means findings do not apply to patients with severe underweight or anorexia nervosa comorbidity.
Mechanistic rationale
– ICBT can deliver behavioral activation, structured food scheduling, cognitive restructuring, and exposure-based elements effectively in a modular format. Therapist guidance likely contributes to adherence, personalization, and therapeutic alliance—factors associated with better outcomes compared with unguided digital interventions.
Policy and implementation implications
– The trial supports integrating therapist-guided ICBT into clinical pathways as a scalable adjunct to usual care in Japan and potentially other East Asian settings.
– Health systems should consider training therapists for remote guidance, quality assurance mechanisms, and infrastructure for secure delivery and monitoring.
Conclusion
This randomized clinical trial demonstrates that a culturally adapted, therapist-guided ICBT program delivered over 12 weeks produced a clinically meaningful reduction in weekly combined binge eating and compensatory episodes among women with bulimia nervosa in Japan compared with usual care. The moderate-to-large effect size and reported acceptability indicate that guided ICBT is a feasible option to expand access to evidence-based care for bulimia nervosa in regions with limited CBT availability.
However, key gaps remain: confirmation in larger and more diverse populations (including men and younger adolescents), direct comparisons with face-to-face CBT and unguided digital interventions, and assessment of long-term durability are necessary before broad policy change. Clinicians and health systems should weigh the benefits of improved access and early efficacy against the need for ongoing monitoring and stepped-care integration.
References
Hamatani S, Matsumoto K, Andersson G, Sato Y, Fukudo S, Sudo Y, Hirano Y, Ino K, Ishibashi T, Tomioka Y, Umehara H, Numata S, Nakamura M, Otani R, Sakuta R, Sekiguchi A, Kosaka H, Mizuno Y; HOPE Project Consortium; Kamashita R, Yoshida T, Matsuura K, Tomari S, Funaba M, Sasaki N, Sako H, Shimada S, Inoue T. Guided Internet-Based Cognitive Behavior Therapy for Women With Bulimia Nervosa: A Randomized Clinical Trial. JAMA Netw Open. 2025 Aug 1;8(8):e2525165. doi: 10.1001/jamanetworkopen.2025.25165 IF: 9.7 Q1 . PMID: 40762916 IF: 9.7 Q1 ; PMCID: PMC12326282 IF: 9.7 Q1 .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Publishing; 2013.- Fairburn CG. Cognitive behavior therapy and eating disorders. Behaviour Research and Therapy. 2008;46(5):532–544.