Introduction
Systemic lupus erythematosus (SLE) is a complex autoimmune disease characterized by multi-organ inflammation and significant morbidity. Despite advances in immunosuppressive therapies, many patients continue to experience flares and chronic disease activity, underscoring the necessity for targeted biologic treatments. Recent attention has focused on cytokine pathways involved in B-cell survival and autoantibody production, notably B-lymphocyte stimulator (BLyS) and proliferation-inducing ligand (APRIL). Telitacicept, a novel dual inhibitor of these cytokines, has shown promise in earlier-phase studies, warranting further investigation in a rigorous phase 3 trial.
Study Design
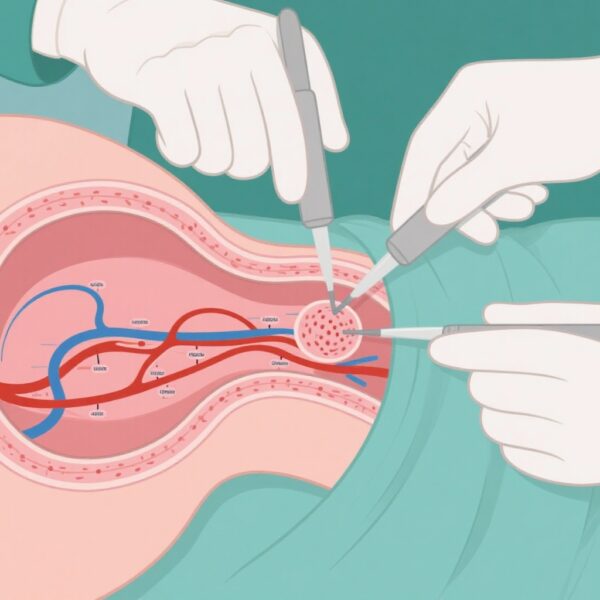
This randomized, double-blind, placebo-controlled phase 3 trial was conducted across multiple centers in China, enrolling adults with active SLE despite standard therapy. Patients were randomly assigned in a 1:1 ratio to receive 160 mg of subcutaneous telitacicept or placebo weekly for 52 weeks, alongside their ongoing background treatments, including corticosteroids, immunosuppressants, and antimalarials. The primary efficacy endpoint was the proportion of patients achieving a response on the modified SLE Responder Index 4 (SRI-4) at week 52. This composite measure mandated a reduction of at least 4 points on the SELENA-SLEDAI score, no new disease activity as per the British Isles Lupus Assessment Group index, and no worsening in the Physician’s Global Assessment (PGA). Secondary endpoints included the proportion of patients with a ≥4 point reduction in SELENA-SLEDAI and evaluations of safety parameters.
Key Results and Efficacy
Out of 433 screened participants, 335 were randomized—167 received telitacicept and 168 placebo. At week 52, the trial demonstrated a statistically significant benefit of telitacicept: 67.1% of patients in the treatment group achieved the primary SRI-4 response compared to 32.7% in the placebo group (adjusted difference 34.5 percentage points; 95% CI, 24.3 to 44.7; P<0.001). Additionally, a ≥4 point reduction in SELENA-SLEDAI was observed in 70.1% of the telitacicept group versus 40.5% of placebo recipients (difference 29.6%; 95% CI, 13.1 to 46.1). These findings suggest a substantial clinical benefit in reducing disease activity among patients receiving telitacicept.
Safety Profile and Adverse Events
While demonstrating efficacy, telitacicept was associated with a higher incidence of certain adverse events. Overall, 74.9% of the telitacicept group experienced adverse events deemed related to the treatment, compared to 50.0% in the placebo group. Notably, upper respiratory tract infections occurred more frequently in the telitacicept group (31.7% vs. 19.0%), alongside reductions in immunoglobulin G (15.6% vs. 1.2%) and M (15.0% vs. 0.6%) levels. Injection-site reactions were also more common with telitacicept (12.6% vs. 0.6%). These findings underscore the importance of monitoring immunoglobulin levels and infectious complications during therapy.
Discussion
The results underscore telitacicept’s potential as an effective targeted biologic in the management of active SLE. Its mechanism—dual blockade of BLyS and APRIL—aims directly at B-cell survival pathways, which are central to SLE pathogenesis. The significant improvements in disease activity measures reflect the biological plausibility of cytokine inhibition. However, the increased risk of infections and hypogammaglobulinemia warrants careful patient selection and vigilant monitoring. These results align with previous phase 2 studies, advancing telitacicept’s development as a promising therapeutic option.
Limitations and Future Directions
While encouraging, the study’s limitations include its restriction to Chinese populations and the relatively short duration for assessing long-term safety. Further studies should explore the efficacy of telitacicept across diverse ethnic groups, examine optimal dosing strategies, and evaluate long-term outcomes and safety. Integration into clinical practice will also require stratification of patients who would most benefit, balancing efficacy with potential immunosuppression risks.
Conclusion
This phase 3 trial provides compelling evidence supporting telitacicept as a novel targeted therapy for active SLE, demonstrating substantial improvements in disease activity with an acceptable safety profile under close monitoring. The findings may influence future treatment algorithms and herald a new era of biologic interventions focusing on specific cytokine pathways integral to SLE pathogenesis.
Funding and Trial Registration
The trial was funded by RemeGen and is registered under ClinicalTrials.gov number NCT04082416.