Highlights
- Adolescents with higher clinic or ambulatory blood pressure exhibit more subclinical cardiovascular injury markers.
- Ambulatory blood pressure phenotypes—white-coat, masked, and sustained hypertension—are all associated with increased target organ injury risk compared to normotensive peers.
- Findings underscore the need for early risk stratification and potential intervention in adolescent hypertension, even before clinical disease manifests.
Study Background and Disease Burden
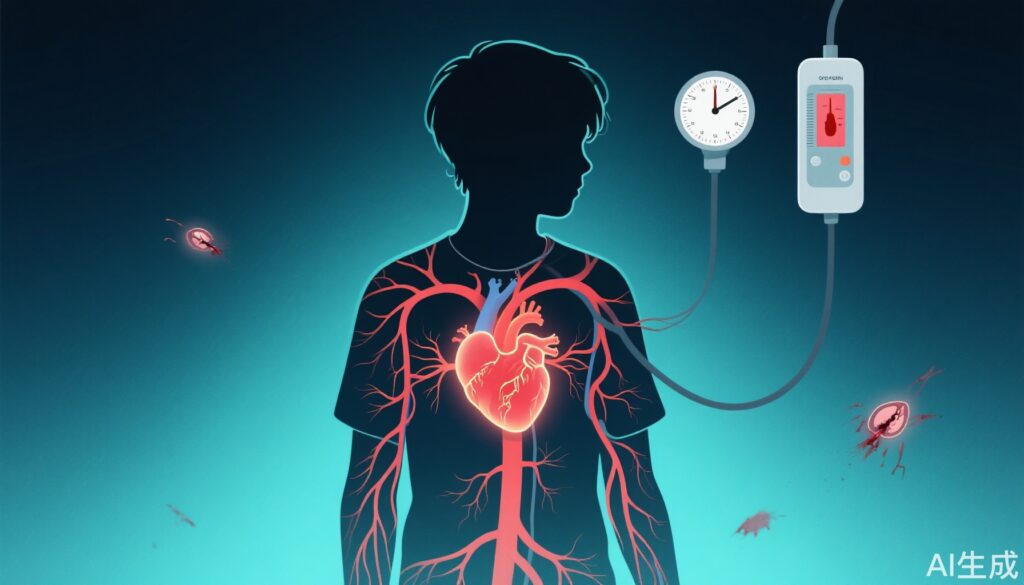
Hypertension is traditionally viewed as an adult disease, but its roots often trace back to adolescence. Globally, the prevalence of elevated blood pressure among youth continues to rise, paralleling increases in childhood obesity and sedentary lifestyles. While overt cardiovascular events are rare in the young, subclinical target organ injury such as increased left ventricular mass, impaired cardiac function, and vascular stiffness can precede symptomatic disease by years. Detecting these early changes is crucial, as they portend a higher risk of adult cardiovascular morbidity and mortality. However, the relationship between varying degrees of blood pressure elevation and the cumulative burden of target organ damage in otherwise healthy adolescents remains poorly defined.
Study Design
The SHIP AHOY (Study of High blood pressure In Pediatrics: Adult Hypertension Onset in Youth) investigators conducted a cross-sectional, multicenter analysis of 244 healthy adolescents (mean age 15.5±1.8 years, 60.1% male). Participants were categorized based on both clinic and ambulatory systolic blood pressure readings into three risk strata: low (90th percentile). Additionally, ambulatory blood pressure patterns were classified as normotensive, white-coat hypertension (elevated clinic BP, normal ambulatory), masked hypertension (normal clinic, elevated ambulatory), or sustained hypertension (elevated in both settings).
Target organ injury was assessed through echocardiographic measurement of left ventricular mass, evaluation of systolic and diastolic cardiac function, and assessment of vascular stiffness. The primary endpoint was the number of target organ injury markers present per participant. Multivariable general linear modeling was employed to adjust for potential confounding variables and to elucidate independent associations.
Key Findings
A striking 47.6% of adolescents in the study exhibited at least one marker of target organ injury, with 16.4% showing two or more. The burden of injury rose with increasing blood pressure percentile:
- Based on clinic BP, the proportion of participants with more than one injury marker was 6.7% (low-risk), 19.1% (mid-risk), and 21.8% (high-risk) (P=0.02).
- For ambulatory BP, these rates were 9.6%, 15.8%, and 32.2%, respectively (P<0.001).
Ambulatory blood pressure phenotype provided further granularity:
- Normotensive: 8% had >1 injury marker
- White-coat hypertension: 23%
- Masked hypertension: 35%
- Sustained hypertension: 32%
All associations remained significant after multivariable adjustment, indicating independent links between blood pressure elevation—regardless of measurement modality—and subclinical cardiovascular injury. Notably, both white-coat and masked hypertension—often considered benign or intermediate states—were associated with a substantially elevated burden of injury markers compared to normotensive peers.
Expert Commentary
These findings challenge longstanding assumptions that mild or transient blood pressure elevations in youth are inconsequential. The robust association between both clinic and ambulatory blood pressure elevations (including white-coat and masked phenotypes) and early organ damage suggests that risk stratification in adolescence should be more nuanced. As Dr. Elaine Urbina, a co-author and expert in pediatric hypertension, has previously noted, “Ambulatory blood pressure monitoring uncovers risk that would otherwise be missed by office measurements alone, highlighting the need for comprehensive assessment in at-risk youth.”
The study’s cross-sectional nature limits causal inference; longitudinal follow-up is necessary to determine whether early intervention can reverse or halt progression of subclinical injury. However, the data reinforce the biological plausibility that sustained hemodynamic stress—even in the absence of symptoms—can initiate maladaptive cardiovascular remodeling processes from a young age.
Conclusion
The SHIP AHOY Study provides compelling evidence that even modest elevations in blood pressure during adolescence are not benign, but rather are associated with a greater cumulative burden of subclinical cardiovascular injury. These findings advocate for early identification and possible intervention in youth with high-normal or mildly elevated blood pressure—even before clinical hypertension is diagnosed. Further research is needed to establish the most effective screening and management strategies, but clinicians should be vigilant in recognizing the spectrum of hypertension phenotypes in adolescents to mitigate long-term cardiovascular risk.
References
1. Hamdani G, Urbina EM, Daniels SR, Falkner BE, Ferguson MA, Flynn JT, Hanevold CD, Ingelfinger JR, Khoury PR, Lande MB, Meyers KE, Samuels J, Mitsnefes M. Youth Blood Pressure and Target Organ Injury Markers: The SHIP AHOY Study. Hypertension. 2025 Jun;82(6):992-1001. doi: 10.1161/HYPERTENSIONAHA.124.23018. Epub 2025 Feb 27. PMID: 40013356; PMCID: PMC12078005.
2. Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
3. Lurbe E, Agabiti-Rosei E, Cruickshank JK, et al. 2016 European Society of Hypertension Guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016 Oct;34(10):1887-1920.