Highlights
- Routine use of cerebral embolic protection (CEP) devices during TAVI does not significantly reduce overall or disabling stroke within 72 hours post-procedure.
- Large registry data suggest potential benefits for selected endpoints, such as major stroke, mortality, and post-procedural outcomes, though effect sizes are modest.
- CEP use is associated with low rates of serious device-related complications and similar vascular access risks to standard TAVI.
- Current evidence does not support routine, universal use of CEP during TAVI, but further research is needed to define high-risk subgroups who may benefit.
Clinical Background and Disease Burden
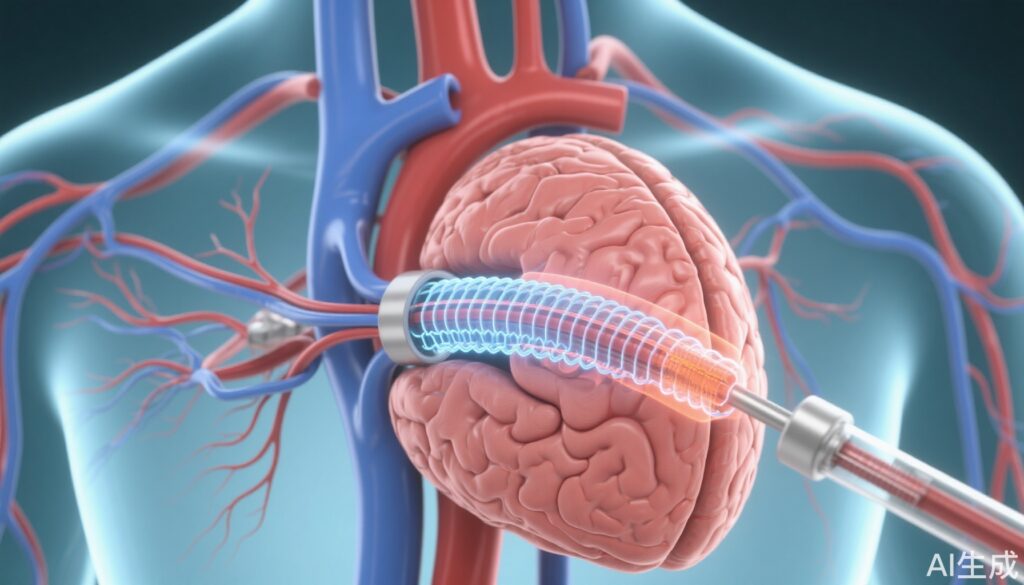
Transcatheter aortic-valve implantation (TAVI) has transformed the management of severe aortic stenosis, offering a minimally invasive option for patients at high or prohibitive surgical risk, and increasingly for lower-risk cohorts. Despite procedural advances, periprocedural stroke remains a feared complication, occurring in approximately 2–4% of cases. Strokes after TAVI are associated with significant morbidity, mortality, prolonged hospitalization, and increased healthcare costs. Embolic debris, released during valve deployment or manipulation, is a principal mechanism. Cerebral embolic protection (CEP) devices aim to capture or deflect such debris, theoretically reducing cerebral infarction and improving neurological outcomes. However, the routine clinical value of CEP remains contentious.
Methodology
The BHF PROTECT-TAVI trial, a multicenter, randomized controlled study conducted across 33 UK centers, enrolled 7,635 patients undergoing TAVI for aortic stenosis. Participants were randomized 1:1 to TAVI with CEP (n=3,815) or without CEP (n=3,820). The primary outcome was stroke within 72 hours post-TAVI or prior to hospital discharge. Secondary outcomes included disabling stroke, mortality, vascular complications, and serious adverse events. The trial was powered to detect clinically meaningful differences in early stroke incidence.
Complementary to this, a large observational analysis from the Nationwide Readmissions Database (2017–2020) assessed 271,804 TAVI procedures in the United States. CEP device use was documented in 7.3% of cases. Outcomes were compared using multivariable logistic regression, focusing on overall and major stroke, mortality, discharge status, length of stay, and readmission rates.
Key Findings
In the BHF PROTECT-TAVI trial, the incidence of the primary outcome—stroke within 72 hours or before discharge—was 2.1% in the CEP group and 2.2% in the control group (risk difference −0.02 percentage points; 95% CI, –0.68 to 0.63; P=0.94). Disabling stroke occurred in 1.2% (CEP) versus 1.4% (control). Mortality rates were comparable (0.8% vs 0.7%). Access-site complications were similar between groups (8.1% vs 7.7%), as were rates of serious adverse events (0.6% vs 0.3%). Thus, routine CEP did not result in a statistically significant reduction in early stroke or major adverse outcomes.
The large US registry study found that CEP use did not significantly reduce overall stroke rates (1.6% vs 1.9%; odds ratio [OR], 0.95; 95% CI, 0.84–1.07; P=0.364), but was associated with a modest yet statistically significant reduction in major stroke (1.2% vs 1.5%; OR, 0.85; 95% CI, 0.74–0.98; P=0.02). CEP use also correlated with shorter hospital stays, higher rates of discharge to home or self-care (74.9% vs 70.6%), lower in-hospital mortality (0.7% vs 1.3%), and reduced 30- and 180-day readmission rates. Patients with prior valve surgery were at the highest risk for stroke.
Mechanistic Insights and Biological Plausibility
CEP devices are designed to prevent embolic debris generated during TAVI from reaching the cerebral circulation. Histopathological studies and MRI data confirm that debris is often captured by CEP devices and that silent cerebral embolization is frequent. However, the translation of these surrogate findings into meaningful reductions in clinical stroke remains unproven in most large randomized controlled trials. The marginal reduction in major stroke observed in registry data may reflect benefit in selected patient subgroups or differences in event adjudication and definitions.
Expert Commentary
Current international guidelines (AHA/ACC, ESC/EACTS) do not recommend routine CEP use during TAVI, citing insufficient evidence for broad clinical efficacy. Expert consensus suggests that CEP may be considered in highly selected patients with elevated stroke risk, such as those with prior cerebrovascular events, extensive aortic arch atheroma, or prior valve surgery. Ongoing research is needed to refine patient selection and optimize device design and procedural technique.
Controversies and Limitations
Several limitations warrant consideration:
- The BHF PROTECT-TAVI trial was rigorously conducted but may not be generalizable to all healthcare settings or device types.
- Stroke events are relatively infrequent, necessitating very large sample sizes for sufficient statistical power.
- Registry data are observational and subject to confounding, despite statistical adjustment.
- Potential benefits of CEP may be underestimated if only high-risk patients derive benefit—subgroup analyses and biomarker studies are ongoing.
- Cost-effectiveness and real-world device deployment logistics remain to be fully elucidated.
Conclusion
Routine use of cerebral embolic protection during TAVI does not significantly reduce the incidence of periprocedural stroke in unselected patients. While registry data suggest possible benefits for major stroke and secondary endpoints, these findings do not currently justify universal CEP deployment. Thoughtful patient selection, further risk stratification, and ongoing innovation in device technology and procedural strategy are needed. Future research should focus on identifying high-risk populations who may derive greater benefit from cerebral protection.
References
1. Kharbanda RK, Kennedy J, Jamal Z, et al; BHF PROTECT-TAVI Investigators. Routine Cerebral Embolic Protection during Transcatheter Aortic-Valve Implantation. N Engl J Med. 2025 Jun 26;392(24):2403-2412. doi: 10.1056/NEJMoa2415120 IF: 78.5 Q1 .2. Shekhar S, Isogai T, Agrawal A, et al. Outcomes and Predictors of Stroke After Transcatheter Aortic Valve Replacement in the Cerebral Protection Device Era. J Am Heart Assoc. 2024 Aug 6;13(15):e034298. doi: 10.1161/JAHA.124.034298 IF: 5.3 Q1 .3. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease. J Am Coll Cardiol. 2021;77(4):e25-e197.
4. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561-632.