Highlight
- RESCUE was a randomized, double-blind, placebo-controlled phase 2 trial evaluating RNS60 as an adjunct therapy in large vessel occlusion (LVO) acute ischemic stroke patients undergoing endovascular thrombectomy.
- RNS60 was safe and well tolerated with no increase in serious adverse events or mortality compared with placebo.
- The higher dose of RNS60 (1.0 mL/kg/h) reduced infarct volume growth by 47% at 48 hours after thrombectomy versus placebo.
- Although other functional outcomes did not reach statistical significance, trends suggested improved neurological recovery and functional independence favoring RNS60 1.0 mL/kg/h at 90 days.
Study Background and Disease Burden
Acute ischemic stroke (AIS) due to large vessel occlusion (LVO) carries substantial morbidity and mortality despite advances such as timely endovascular thrombectomy (EVT) and intravenous thrombolysis. Early reperfusion is critical to improve outcomes; however, a considerable number of patients experience poor neurological recovery and disability even after successful EVT.
Currently, no adjunct neuroprotective therapies are approved to mitigate ischemic brain injury or secondary infarct progression during and after reperfusion. This unmet clinical need has driven interest in agents with cerebroprotective properties that can complement mechanical reperfusion strategies.
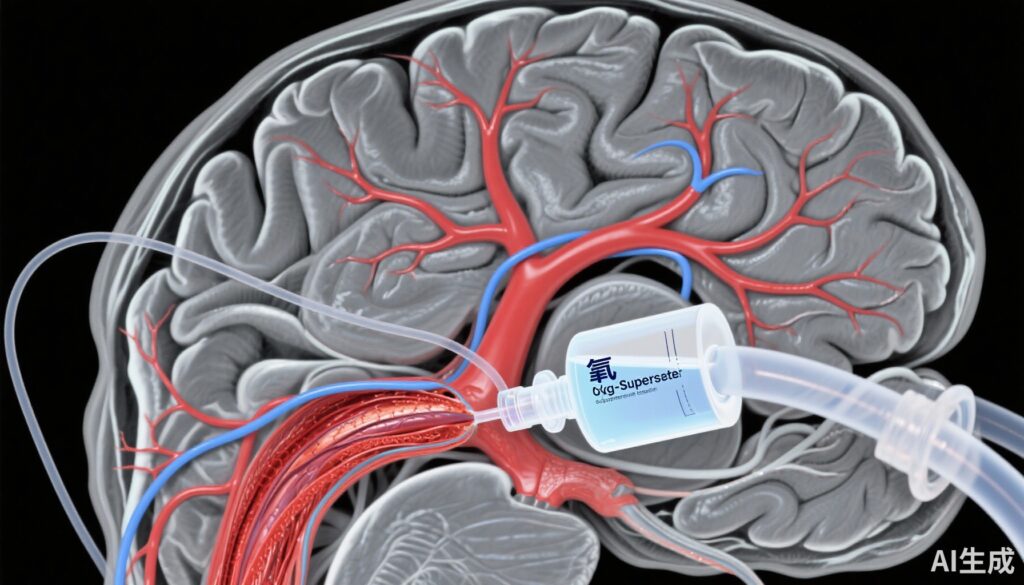
RNS60 is a proprietary saline solution supersaturated with oxygen, developed to exert cerebroprotective and immunomodulatory effects. Experimental models in rodents and nonhuman primates demonstrated RNS60’s ability to reduce infarct size, enhance neuronal survival, and modulate inflammatory responses after ischemic stroke. These preclinical data provided the rationale for clinical evaluation of RNS60 as adjunctive therapy in AIS patients undergoing EVT.
Study Design
The RESCUE trial (NCT04693715) was a randomized, multicenter, double-blind, placebo-controlled, phase 2 proof-of-concept study. It enrolled 82 patients with acute ischemic stroke due to LVO treated with EVT, with or without prior intravenous thrombolysis.
Participants were randomized 1:1:1 to receive a 48-hour intravenous infusion of either RNS60 at 0.5 mL/kg/hour, RNS60 at 1.0 mL/kg/hour, or placebo at 1.0 mL/kg/hour. The treatment infusion was initiated shortly after EVT.
The primary safety endpoints were rates of serious adverse events (SAEs) and mortality over 90 days. Efficacy outcomes included change in infarct volume measured by imaging at 48 hours, neurological deficits assessed by the National Institutes of Health Stroke Scale (NIHSS), functional disability assessed by the modified Rankin Scale (mRS) and Barthel Index at 90 days, stroke worsening, and health-related quality of life measured by the EuroQoL scale.
Key Findings
Safety profiles were comparable across treatment arms. SAEs occurred in 33.3% of patients receiving RNS60 0.5 mL/kg/h, 25.0% receiving RNS60 1.0 mL/kg/h, and 28.6% in the placebo group. Mortality rates were lower in the RNS60 groups (6.7% for 0.5 mL/kg/h, 8.3% for 1.0 mL/kg/h) than placebo (14.3%). No safety signals or unexpected adverse events were reported.
The higher-dose RNS60 group demonstrated a significant 47% reduction in infarct volume growth at 48 hours post-EVT versus placebo (median 21.4 mL [IQR 5.0–29.1] vs 40.6 mL [IQR 6.3–62.3]; P<0.05). This reflects potential neuroprotection against secondary ischemic injury after reperfusion.
Neurological and functional outcome assessments favored RNS60 1.0 mL/kg/h but did not achieve statistical significance. The proportion of patients with favorable functional outcomes (mRS 0–2) and functional independence (Barthel Index ≥95) was numerically higher in the higher-dose group at day 90. The NIHSS and EuroQoL scores showed similar trends.
No significant difference was observed in stroke worsening events between groups.
Overall, the results confirm safety and suggest a dose-dependent efficacy signal, especially in infarct volume attenuation, supporting further investigation.
Expert Commentary
The RESCUE study provides important proof-of-concept data for the emerging paradigm of adjunct neuroprotection combined with reperfusion in LVO AIS. The reduction in infarct growth—a surrogate marker linked to clinical outcomes—indicates RNS60 has biological activity that could translate into improved recovery.
As a proprietary oxygen-enriched saline, RNS60 may exert multiple beneficial mechanisms including enhanced tissue oxygenation, reduction of reperfusion injury, and modulation of inflammatory cascades known to exacerbate ischemic damage. The absence of increased adverse events addresses concerns about potential oxidative stress or other complications.
Limitations include the relatively small sample size, which limited power for clinical endpoints, and the single-phase 2 design. Larger, adequately powered phase 3 trials are needed to confirm efficacy on functional outcomes. Heterogeneity in baseline stroke severity and treatment variables also warrants stratified analyses.
These findings align with calls for adjunct therapies targeting ischemia-reperfusion injury and support innovative treatment strategies beyond rapid vessel recanalization alone.
Conclusion
The RESCUE trial demonstrated that adjunctive RNS60 therapy in acute ischemic stroke patients undergoing endovascular thrombectomy is safe and reduces infarct volume growth, particularly at the 1.0 mL/kg/hour dosing. Although clinical outcomes were not statistically significant, trends toward improved disability and independence encourage further phase 3 studies to validate these promising signals.
RNS60 offers a novel approach to neuroprotection leveraging oxygen supersaturated saline, potentially addressing the unmet need for adjunctive stroke therapies. Continued research is essential to establish its role in clinical practice and improve outcomes for patients with large vessel occlusion stroke.