Highlights
1. AI-driven model achieves high accuracy in evaluating ankylosing spondylitis severity from X-ray images.
2. Automated spine point detection and mSASSS assessment streamline clinician workflow and minimize inter-observer variability.
3. The model identifies severe structural changes (mSASSS score 3) with 97.4% accuracy, demonstrating robust potential for clinical application.
Study Background and Disease Burden
Ankylosing spondylitis (AS) is a chronic inflammatory rheumatic disease primarily affecting the spine and sacroiliac joints, leading to progressive structural damage, impaired mobility, and reduced quality of life. Timely and accurate assessment of disease severity is crucial for therapeutic decision-making, prognostication, and monitoring response to treatment. Traditional evaluation relies on radiographic scoring systems such as the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS), which, despite its clinical value, is time-consuming and subject to inter-observer variability. Given the increasing prevalence of AS and limited rheumatology workforce in many settings, there is an urgent need for automated, reproducible, and scalable solutions to support the efficient management of this disease.
Study Design
This prospective, AI-driven modeling study by Chen et al. (Ann Med. 2025) aimed to develop and validate an automated severity inspection model for AS, leveraging X-ray images and mSASSS. The study included X-rays from 222 patients, manually annotated by three expert readers according to the gold standard for mSASSS scoring. The AI model was designed in two stages:
1. Keypoint Detection: Automatic identification of anatomical landmarks along the spine.
2. mSASSS Evaluation: Classification of vertebral patches based on mSASSS criteria.
The model’s accuracy was compared with consensus expert ratings. The study followed ethical principles in accordance with the Declaration of Helsinki.
Key Findings
The two-stage AI model exhibited remarkable technical performance:
– **Stage 1: Keypoint Detection**
– The mean error distance between AI-predicted and ground truth spine points was only 1.57 micrometres, signifying precise anatomical localization.
– **Stage 2: mSASSS Evaluation**
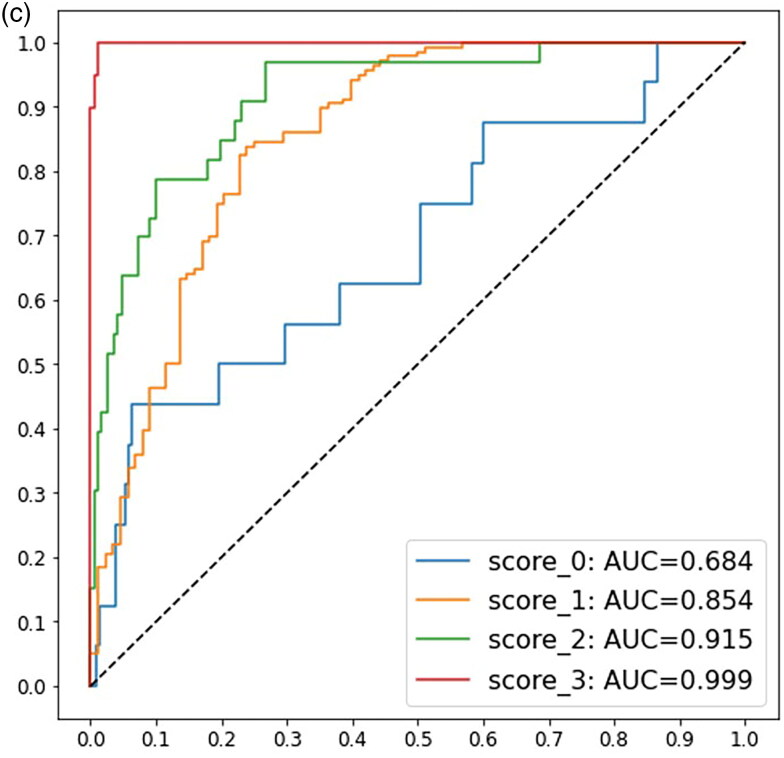
– The classification network achieved a mean accuracy of 0.81 (81%) in assigning mSASSS grades to vertebral patches.
– Notably, the model correctly identified 97.4% of patches corresponding to advanced structural damage (mSASSS score 3), while patches rated as score 0 (no damage) were sometimes misclassified as 1 or 2, indicating a tendency for overestimation in the lower score range.
These findings suggest that the AI model is especially robust in detecting severe structural alterations, a critical aspect for clinical decision-making regarding advanced disease. The model’s high reproducibility and speed have the potential to standardize assessments, reduce clinician workload, and facilitate large-scale epidemiological or interventional studies.
Expert Commentary
The integration of artificial intelligence into musculoskeletal radiology is a transformative step for rheumatology. The model’s robust performance in detecting higher mSASSS grades is particularly valuable, as these represent clinically significant spinal damage associated with poor functional outcomes. However, the slight misclassification at the lower end of the mSASSS spectrum highlights the need for further refinement, possibly through model retraining with larger, more diverse datasets and incorporation of additional imaging modalities such as MRI.
From a clinical perspective, automated scoring could dramatically reduce the time and expertise needed for radiographic evaluation, especially in resource-limited settings or high-volume clinics. Furthermore, AI-driven standardization may improve inter-rater reliability, a known limitation of manual mSASSS scoring, and support more consistent monitoring of disease progression and therapeutic response.
Nevertheless, clinicians should be aware of the model’s limitations, including its current reliance on high-quality, standardized X-rays and its performance in distinguishing early structural changes. Integration into clinical practice will require rigorous external validation, regulatory approval, and user-friendly interfaces tailored to real-world workflow.
Conclusion
The AI-based severity inspection model for ankylosing spondylitis developed by Chen et al. represents a significant advancement in radiographic disease assessment. By automating keypoint detection and mSASSS scoring with high accuracy, the model offers an efficient, reproducible, and scalable tool to assist clinicians in grading AS severity. Future work should focus on expanding validation across diverse patient populations and clinical environments, and on integrating AI models into rheumatology practice to maximize their translational impact. The ultimate goal is to enhance patient care through rapid, objective, and standardized evaluation of disease burden.
References
Chen CW, Tsai HH, Yeh CY, Yang CK, Tsou HK, Leong PY, Wei JC. Application of Artificial Intelligence in rheumatic disease classification: an example of ankylosing spondylitis severity inspection model. Ann Med. 2025 Dec;57(1):2512131. doi: 10.1080/07853890.2025.2512131 .
Additional relevant literature:
– van der Heijde D, et al. How to read radiographs according to the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS). Ann Rheum Dis. 2004;63(10):1186-1193.
– Pedersen SJ, et al. Recent advances in imaging in axial spondyloarthritis. Curr Opin Rheumatol. 2020;32(4):361-368.