Highlight
- New classification of myocardial infarction differentiates spontaneous, secondary, and no myocardial infarction in patients initially diagnosed with Type 2 MI.
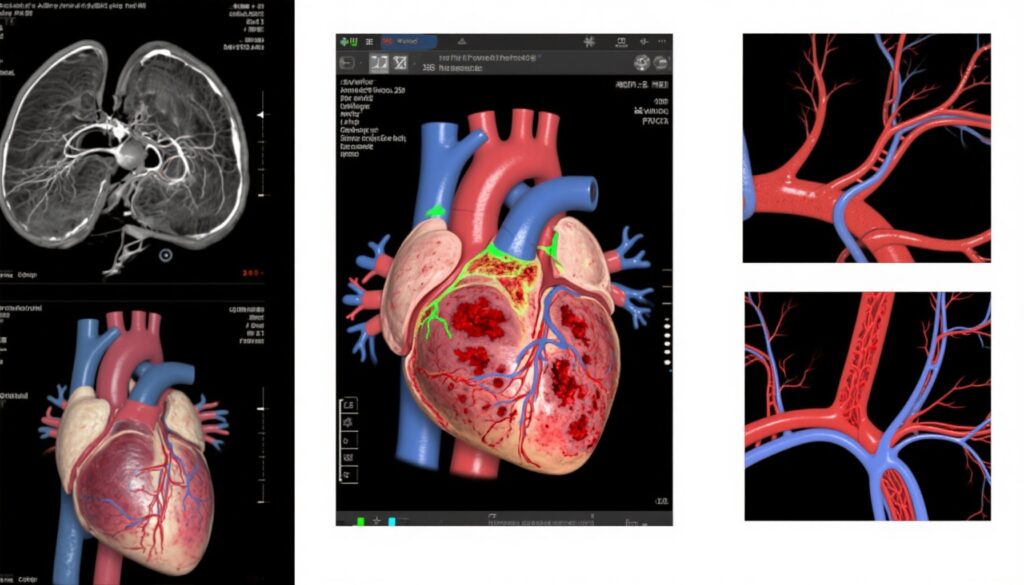
- Cardiac imaging using coronary angiography and cardiac magnetic resonance imaging enhances diagnostic specificity beyond traditional clinical criteria.
- Secondary MI patients exhibit higher adverse outcomes, emphasizing the role of imaging-driven reclassification in targeting high-risk groups.
- The refined classification reduces overdiagnosis of MI in acute illness and facilitates appropriate management strategies.
Study Background and Disease Burden
Acute myocardial infarction (MI) is a leading cause of morbidity and mortality worldwide, with substantial clinical heterogeneity. The Type 2 myocardial infarction classification, characterized by myocardial injury due to supply-demand mismatch without acute coronary thrombosis, encompasses a broad and heterogeneous patient population. This heterogeneity complicates clinical decision-making, as the diagnosis currently relies on clinical judgment, cardiac biomarkers, and electrocardiographic changes, often without clear therapeutic pathways. Misclassification may lead to inappropriate management, either under-treatment or overtreatment. Thus, there is a pressing need to develop more objective and precise diagnostic criteria to refine MI subtypes, improve prognostication, and guide treatment, particularly leveraging advanced cardiac imaging modalities.
Study Design
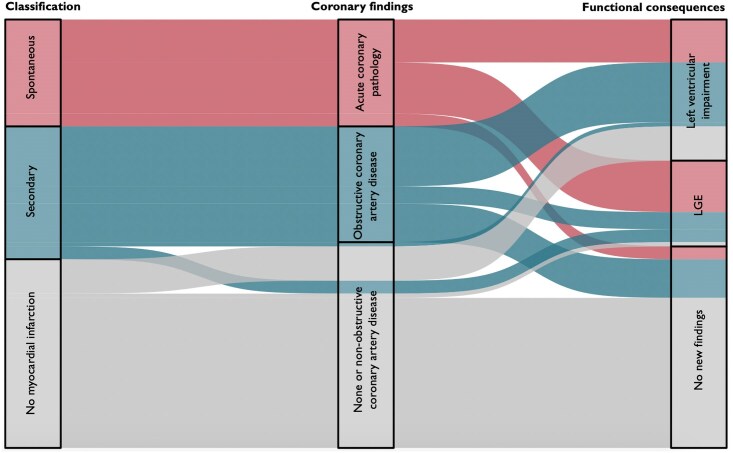
This prospective cohort study was conducted between January 2018 and October 2020, enrolling 108 patients who fulfilled the clinical diagnostic criteria for Type 2 myocardial infarction. Eight patients either withdrew consent or did not complete the investigations, yielding a final study cohort of 100 patients (median age 65 [55–74], 43% female). All patients underwent coronary angiography along with either cardiac magnetic resonance imaging (MRI) or echocardiography. Using these imaging results alongside clinical data, a new classification system was applied to categorize patients into:
(i) Spontaneous myocardial infarction due to acute coronary pathology (e.g., atherothrombosis, coronary embolism, spontaneous coronary dissection, vasospasm).
(ii) Secondary myocardial infarction precipitated by acute illness with presence of obstructive coronary artery disease or evidence of new regional wall motion abnormalities or infarct-pattern myocardial scarring.
(iii) No myocardial infarction defined by absence of obstructive coronary artery disease and no new myocardial abnormality on imaging.
The primary endpoints included accurate classification of MI type, clinical features correlation, and follow-up assessment of adverse cardiovascular outcomes over a median of 4.4 years.
Key Findings
Application of the new classification model significantly reclassified the cohort: 25 patients were identified with spontaneous myocardial infarction, 31 with secondary myocardial infarction, and 44 were reclassified as having no myocardial infarction despite initial clinical Type 2 MI diagnosis.
Demographically, patients with secondary MI were older, exhibited more cardiovascular risk factors, had higher peak cardiac troponin levels, and a greater history of prior MI, compared to those without myocardial infarction. Conversely, spontaneous MI cases were younger and less likely to have established risk factors.
Clinically, chest pain and electrocardiographic ischemia were common but non-discriminatory between secondary and non-MI groups, whereas spontaneous MI patients predominantly reported chest pain (92%) with universal ECG ischemia evidence. Troponin concentrations were markedly elevated in both spontaneous and secondary MI groups compared to no MI (median max troponin 6451 ng/L and 1522 ng/L versus 578 ng/L; P < 0.001).
Imaging modalities facilitated definitive diagnosis: 96% of spontaneous MI patients underwent invasive coronary angiography, while CT coronary angiography was used in 42% and 55% of secondary MI and no MI groups, respectively. Cardiac MRI was performed in approximately 78% of patients equally across groups, supplementing echocardiography when MRI was not feasible.
Acute coronary pathology identified in spontaneous MI included acute atherothrombosis, coronary embolism, spontaneous coronary dissection, and vasospasm. Secondary MI was primarily characterized by obstructive coronary artery disease (87%). Patients classified as no MI lacked obstructive disease but half had non-obstructive coronary artery disease without infarction evidence.
Longitudinal follow-up revealed markedly higher adverse outcomes in secondary MI patients, with 55% experiencing death, recurrent MI, or heart failure hospitalizations, significantly greater than the no MI group (16%, P < 0.001).

Expert Commentary
The heterogeneity inherent in Type 2 MI diagnostic criteria has historically challenged clinicians owing to overlapping clinical and biochemical features between MI subtypes and mimic conditions. This study demonstrates that integrating advanced cardiac imaging into the diagnostic framework can meaningfully stratify patients, identifying those with true spontaneous MI requiring focused coronary interventions, secondary MI necessitating management of underlying acute illness and ischemic heart disease, and patients without MI who may benefit from alternative diagnostic considerations.
Notably, similarities in chest pain prevalence and ECG changes between secondary MI and no MI groups underscore the limitations of symptom-based criteria and highlight the indispensability of imaging for diagnostic clarity. Elevated troponin remains a hallmark but is insufficient alone to delineate MI subtype.
By distinguishing these groups, this classification may optimize resource allocation, reduce unnecessary invasive procedures, and target therapies to high-risk subsets, thereby improving outcomes.
However, limitations include the single-cohort design and referral bias to tertiary centers with advanced imaging capabilities, which may restrict generalizability. Further validation in broader multicenter settings is warranted.
Conclusion
The implementation of a new clinical classification of acute myocardial infarction, guided by coronary angiography and cardiac magnetic resonance imaging or echocardiography, enhances diagnostic precision beyond conventional Type 2 MI criteria. This approach substantially reduces overdiagnosis of MI in acute illness and identifies patients at elevated risk of adverse cardiovascular events. Incorporation of this classification into clinical practice could refine therapeutic decision-making, fostering tailored management strategies that improve patient outcomes.
References
Boeddinghaus J, Bularga A, Taggart C, Wereski R, McDermott M, Thurston AJF, Ferry AV, Williams MC, Baker AH, Dweck MR, Newby DE, Chapman AR, Lindahl B, Mills NL; DEMAND-MI Investigators. Implications of a new clinical classification of acute myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2025 Mar 22;14(3):131-141. doi: 10.1093/ehjacc/zuaf002 IF: 4.6 Q1 . PMID: 39824208 IF: 4.6 Q1 ; PMCID: PMC11929527 IF: 4.6 Q1 .
ClinicalTrials.gov Identifier: NCT03338504