Highlight
1. Intravenous tenecteplase showed a neutral effect on 90-day functional outcomes in minor ischemic stroke patients categorized as having disabling deficits based on NIHSS.
2. Patients with disabling symptoms had higher NIHSS scores and presented later with longer onset-to-treatment times.
3. Standard NIHSS-based definitions of disabling stroke did not modify treatment response to tenecteplase.
4. Findings suggest reevaluating intravenous thrombolysis criteria for minor disabling strokes.
Study Background
Minor ischemic strokes, defined by low National Institutes of Health Stroke Scale (NIHSS) scores typically ranging from 0-5, represent a considerable proportion of acute ischemic stroke presentations. These strokes often involve mild neurological deficits but vary in their clinical impact, especially when symptoms are disabling. Current stroke treatment guidelines offer mixed recommendations regarding intravenous thrombolysis in minor stroke, particularly when disabling deficits are present. Tenecteplase, a genetically engineered tissue plasminogen activator with a longer half-life and ease of administration, has been investigated as a thrombolytic agent alternative to alteplase. However, the benefit of tenecteplase specifically in minor disabling stroke remains unclear, necessitating further investigation.
Study Design
The TEMPO-2 trial, a multicenter, randomized clinical trial, enrolled patients with minor ischemic stroke (NIHSS score 0-5) and documented intracranial arterial occlusion within 12 hours of symptom onset. Conducted across 48 global sites from April 2015 to January 2024, the trial randomized participants to intravenous tenecteplase (0.25 mg/kg) or nonthrombolytic standard care, with functional follow-up at 90 days. This secondary analysis stratified patients based on disabling versus nondisabling neurological deficits assessed by NIHSS score definitions endorsed by the TREAT Task Force consensus. Additional definitions from the ARAMIS and NINDS trials were also evaluated. The primary outcome was return to baseline pre-stroke modified Rankin Scale (mRS) score at 90 days, an indicator of functional recovery.
Key Findings
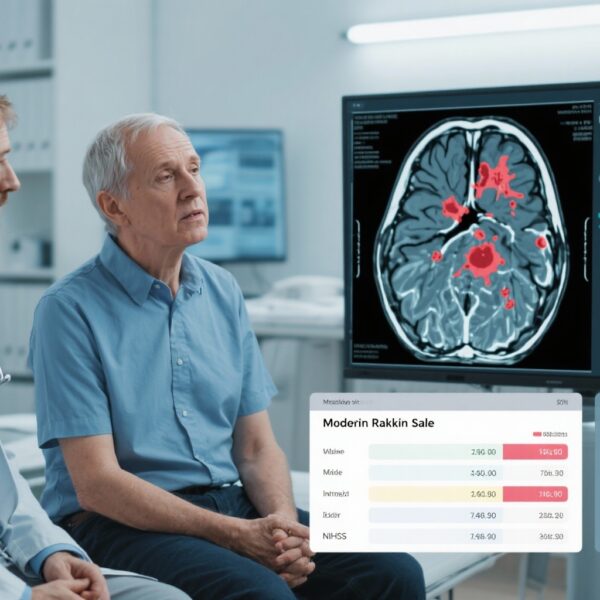
Among 884 analyzed patients (median age 72 years; 41.7% women), 100 (11.3%) presented with disabling deficits. Compared to the nondisabling group, those with disabling symptoms had significantly higher median NIHSS scores (4 vs 2), later hospital arrival times (median 288 vs 133 minutes), and prolonged onset-to-treatment intervals (411 vs 278 minutes), signifying delayed intervention.
In the disabling stroke cohort, the proportion achieving the primary outcome was 54.7% (29/53) in the tenecteplase group and 68.1% (32/47) in the standard care group. The adjusted risk ratio (aRR) was 0.81 (95% CI, 0.60–1.10), indicating no statistically significant benefit. Similar neutral treatment effects were observed in the nondisabling group (73.9% vs 75.6%; aRR 0.98; 95% CI, 0.91–1.07) with no significant interaction (P = 0.32). These results were consistent across alternate disabling stroke definitions.
The data suggest that intravenous tenecteplase does not confer improved functional recovery at 90 days in minor ischemic stroke patients, regardless of baseline symptom disabling status as defined by NIHSS criteria. Importantly, patients with disabling deficits in TEMPO-2 presented later and received treatment later, factors that may influence thrombolysis effectiveness.
Expert Commentary
The neutral findings contrast with prior assumptions that disabling symptoms in minor stroke should prompt thrombolysis to improve outcomes. The prolonged delay in treatment observed among disabling stroke patients may have attenuated potential benefits of thrombolysis, emphasizing the critical role of early intervention. Additionally, the reliance on NIHSS-based scores to define disabling deficits may oversimplify the clinical heterogeneity in minor stroke presentations, limiting the precision of patient selection for thrombolysis.
Current guideline recommendations for thrombolysis in minor disabling stroke vary, reflecting the paucity of robust evidence. The TEMPO-2 secondary analysis contributes valuable data urging reexamination of eligibility criteria. Further research should consider alternative metrics of symptom disablingness, combine imaging biomarkers, and explore the impact of treatment timing. Additionally, ongoing trials and meta-analyses will provide broader insights into the utility of tenecteplase and other thrombolytics in minor stroke subgroups.
Conclusion
This secondary analysis from the TEMPO-2 trial indicates that intravenous tenecteplase does not improve 90-day functional outcomes in patients with minor ischemic stroke, regardless of NIHSS-defined disabling symptoms. Delayed presentation and treatment may contribute to the observed neutral effects. These findings highlight the need to refine thrombolytic treatment strategies and reconsider current NIHSS-based definitions of disabling stroke. Personalized approaches incorporating clinical, imaging, and temporal parameters are required to optimize therapy decisions in minor disabling stroke.
Funding and Trial Registration
The TEMPO-2 trial was registered on ClinicalTrials.gov (Identifier: NCT02398656). The funding sources were reported in the original publication but are not detailed here.
References
Zhang Y, Buck BH, Barber PA, et al. Thrombolysis With Tenecteplase for Minor Disabling Stroke: Secondary Analysis of the TEMPO-2 Randomized Clinical Trial. JAMA Neurol. 2025 Oct 27:e254152. doi: 10.1001/jamaneurol.2025.4152. Epub ahead of print. PMID: 41143808; PMCID: PMC12560024.