Highlight
1. PSMA-PET offers superior detection of recurrent prostate cancer lesions, allowing for tailored radiotherapy intensification.
2. PSMA-PET-guided intensification of salvage radiotherapy (PSMAiSRT) after radical prostatectomy significantly improves failure-free survival (FFS) compared to standard-of-care (SOC) salvage radiotherapy.
3. The treatment intensification, guided by PSMA-PET findings, does not increase toxic effects or decrease quality of life.
4. Greatest clinical benefit was observed in patients with PSA levels ≥ 0.3 ng/mL at salvage radiotherapy initiation.
Study Background and Disease Burden
Prostate cancer patients undergoing radical prostatectomy (RP) often face biochemical recurrence (BCR), reflected by rising prostate-specific antigen (PSA) levels, which signifies residual or recurrent disease. Salvage radiotherapy (SRT) targeting the prostate bed is the established treatment to mitigate progression, but optimal radiotherapy (RT) fields and dosage customization remain challenging because conventional imaging fails to reliably localize recurrent lesions. Failures after standard salvage RT suggest occult metastases may go untreated, leading to disease progression.
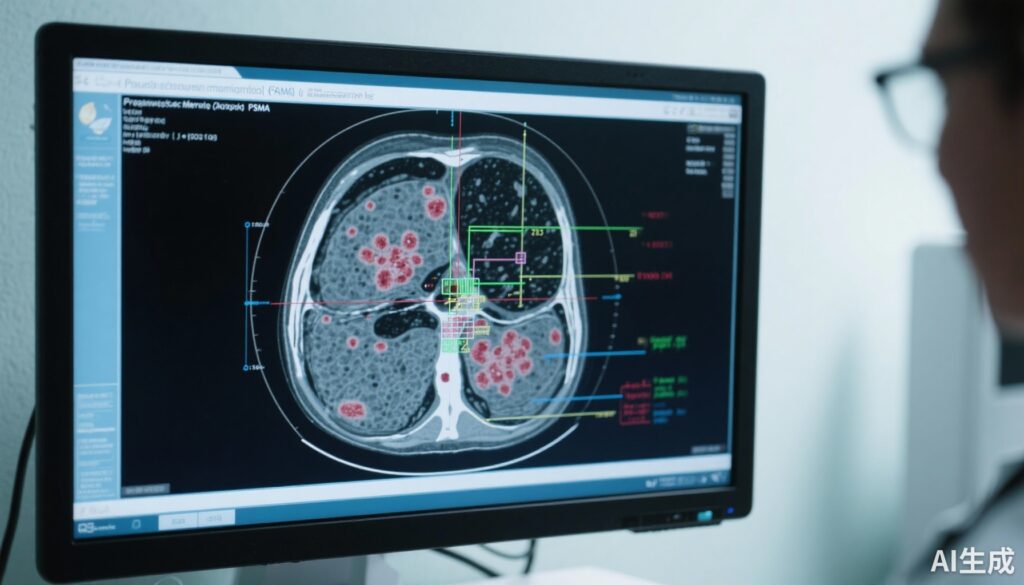
Prostate-specific membrane antigen positron emission tomography (PSMA-PET) has emerged as a highly sensitive and specific imaging modality to detect recurrent prostate cancer lesions at low PSA levels, enabling precise mapping of disease outside the prostate bed. This novel imaging strategy can potentially guide RT intensification targeted to all sites of recurrence, theoretically improving oncologic outcomes. Nevertheless, randomized data demonstrating clinical benefit of PSMA-PET-guided intensification of SRT are lacking.
Study Design
The present study analyzed a stratified cohort from the PSMA-guided intensification of radiotherapy (PSMAgRT) trial, a phase 2, two-center, registry-based randomized clinical trial (ClinicalTrials.gov NCT03525288), conducted from May 2018 to February 2021. It enrolled 130 patients with biochemical recurrence after RP who were eligible for standard salvage RT. Two patients did not proceed to RT, resulting in 128 evaluable participants with a median age of 71 years and PSA at enrollment ranging from 0.1 to 3.0 ng/mL.
Patients were randomized 1:1 to receive either standard-of-care salvage radiotherapy (SOC SRT)—prostate bed RT with optional elective pelvic RT and adjuvant hormonal therapy (HT)—or PSMA-PET/CT-guided SRT intensified to all detected sites of disease. Intensification included pelvic RT, metastasis-directed RT, lymph node boosts, or prostate bed boosts according to PSMA-PET findings. Both study arms had similar utilization rates of adjuvant HT (approximately 85%).
The primary endpoint was failure-free survival (FFS), which encompassed PSA progression (PSA nadir >0.2 ng/mL), radiological progression, initiation of next-line therapy, or death. Secondary endpoints included eugonadal FFS and toxicity profiles over a median follow-up of 37 months (range 7-60 months).
Key Findings
In the PSMAiSRT arm, 52% of patients underwent intensification based on PSMA-PET mapping. The interventions included pelvic RT in 25%, metastasis-directed RT in 3%, lymph node boosts in 30%, and prostate bed boosts in 23% of patients. Adjuvant hormone therapy usage was balanced between the groups.
PSMAiSRT significantly improved FFS compared with SOC SRT (hazard ratio [HR], 0.50; 95% confidence interval [CI], 0.27-0.94; P = .04), indicating a 50% reduction in failure risk. It also enhanced eugonadal FFS (HR, 0.45; 95% CI, 0.21-0.96; P = .03). Notably, the subgroup with baseline PSA ≥ 0.3 ng/mL derived the greatest benefit, with an 83% reduction in failure risk (HR, 0.17; 95% CI, 0.04-0.79; P = .01).
The PSMAiSRT group experienced fewer next-line treatment events (4 vs. 12 in SOC) with HR 0.32 (95% CI, 0.11-1.02; P = .04), reflecting prolonged disease control and delayed systemic therapy initiation.
Importantly, intensified RT guided by PSMA-PET did not increase genitourinary or gastrointestinal toxicities or adversely impact patient-reported quality of life measures, confirming isotoxicity of the intervention.
Expert Commentary
This randomized controlled trial provides the first high-quality evidence that PSMA-PET-guided intensification of salvage radiotherapy after radical prostatectomy can yield clinically meaningful improvements in failure-free survival without additional toxicity burden. By leveraging superior imaging to tailor RT fields, the approach addresses a critical unmet need in prostate cancer management—optimal localization and eradication of recurrent disease.
The observed benefits are biologically plausible, as PSMA-PET can reveal micrometastatic nodal or distant lesions not captured by conventional imaging, guiding precise dose escalation while sparing uninvolved tissue. The findings also support earlier initiation of PSMA-PET-informed salvage RT, particularly in patients with PSA ≥ 0.3 ng/mL.
Limitations include relatively short median follow-up and the phase 2 single-blinded design. The generalizability to community settings requires confirmation, and phase 3 trial data will further solidify the survival impact and cost-effectiveness of this technology integration. Moreover, long-term functional outcomes remain to be established.
Conclusion
The phase 2 PSMAiSRT trial convincingly demonstrates that PSMA-PET-guided intensification of salvage radiotherapy post-radical prostatectomy improves failure-free survival without compromising safety or quality of life. This isotoxic approach refines prostate cancer salvage therapy by personalizing radiotherapy fields based on high-resolution PSMA-PET imaging, marking a significant advancement in post-prostatectomy management.
Pending confirmatory phase 3 results, adoption of PSMA-PET-guided SRT intensification should be considered in clinical practice to optimize oncologic outcomes for patients experiencing biochemical recurrence.
References
Belliveau C, Saad F, Duplan D, et al. Prostate-Specific Membrane Antigen PET-Guided Intensification of Salvage Radiotherapy After Radical Prostatectomy: A Phase 2 Randomized Clinical Trial. JAMA Oncol. 2025 Oct 2. doi:10.1001/jamaoncol.2025.3746
Emmett L, van Leeuwen PJ, Nandurkar R, et al. Treatment outcomes from 68Ga-PSMA PET/CT-informed salvage radiation treatment in men with rising PSA after radical prostatectomy: Early evidence of improved biochemical outcomes. J Nucl Med. 2017;58(9):1425-1430.
Fendler WP, Calais J, Eiber M, et al. Assessment of 68Ga-PSMA-11 PET accuracy in localizing recurrent prostate cancer: A prospective single-arm clinical trial. JAMA Oncol. 2019;5(6):856-863.