Highlight
– In a 1:2 propensity-matched cohort of 54 patients with olfactory neuroblastoma (ONB), no definitive superiority of proton beam radiotherapy (PBRT) over intensity-modulated radiotherapy (IMRT) was demonstrated for local recurrence-free survival (RFS) or overall survival (OS).
– Rates of grade ≥2 radiation treatment–related adverse events (RTAEs) were similar and low overall (≈20%), with 21% after IMRT and 18% after PBRT.
– Wide confidence intervals around 10-year outcome estimates indicate substantial imprecision; the data should be considered hypothesis-generating and useful for planning prospective studies.
Background and clinical context
Olfactory neuroblastoma (ONB), also known as esthesioneuroblastoma, is a rare sinonasal malignancy arising from olfactory epithelium. Clinical behavior ranges from indolent, locally confined tumors to aggressive disease with cranial base and intracranial extension, nodal metastases, and distant spread. Standard management of resectable ONB typically involves craniofacial resection or endoscopic skull base surgery followed by adjuvant radiotherapy for locally advanced or high-grade tumors to reduce locoregional recurrence and improve disease-specific outcomes.
Intensity-modulated radiotherapy (IMRT) is a widely used photon technique that allows conformal dose delivery to complex targets in the sinonasal region while sparing adjacent critical structures (optic apparatus, brain, brainstem, contralateral nasal structures). Proton beam radiotherapy (PBRT) offers a distinct physical advantage through the Bragg peak, concentrating dose within the target and potentially reducing dose distal to the target. For ONB, PBRT is thought to reduce dose to uninvolved optic nerves, the contralateral orbit, temporal lobes, and hippocampi, theoretically lowering long-term risks of neurocognitive decline, vision loss, and secondary malignancy.
Study design and population
Presented data come from Tang et al., a multicenter propensity score–matched cohort study published in JAMA Otolaryngology–Head & Neck Surgery (2025). The analysis included patients with ONB treated between February 2005 and April 2021 across nine academic tertiary centers in North America. Patients who received adjuvant IMRT or PBRT were matched 1:2 by age, modified Kadish stage, and Hyams histologic grade, yielding a cohort of 54 patients (18 PBRT, 36 IMRT).
Key endpoints were recurrence-free survival (RFS) — including local RFS and any RFS — overall survival (OS), and radiation treatment–related adverse events (RTAEs), defined as Common Terminology Criteria for Adverse Events (CTCAE) grade ≥2 events. Data were analyzed July 2024 to January 2025.
Key findings
Demographics and pathology: The cohort included 54 patients (50% female), mean age 46.2 years (SD 15.4). Most had modified Kadish stage C disease (61%) and 44% had Hyams grade III or IV tumors, indicating a sizable fraction with advanced or high-grade disease.
Toxicity: Overall RTAE rate was 20% (8 of 40 patients with evaluable toxicity data). By modality, 21% (6 of 29) of IMRT-treated patients and 18% (2 of 11) of PBRT-treated patients experienced grade ≥2 RTAEs. The manuscript reports these rates as broadly similar; absolute numbers are small, limiting precise comparison.
Oncologic outcomes: At 10 years, the point estimates were:
- Any RFS: IMRT 63.3% (95% CI, 44.6–89.8); PBRT 37.8% (95% CI, 14.2–100); absolute difference 25.5 percentage points favoring IMRT (95% CI, −17.6 to 68.6).
- Local RFS: IMRT 75.6% (95% CI, 59.8–95.4); PBRT 72.7% (95% CI, 45.2–100); difference 2.9 percentage points (95% CI, −35.9 to 41.7).
- Overall survival: IMRT 61.8% (95% CI, 42.8–89.1); PBRT 57.1% (95% CI, 24.3–100); difference 4.7 percentage points (95% CI, −49.2 to 58.6).
Interpretation: Point estimates do not demonstrate a clear advantage for PBRT over IMRT in local control or long-term survival. One point estimate suggested a possible benefit favoring IMRT for any RFS, but confidence intervals were wide and cross both clinically meaningful benefit and harm. The authors appropriately conclude that estimates are imprecise and no definitive comparative effectiveness conclusions can be drawn.
Expert commentary and mechanistic considerations
Biophysical rationale: PBRT’s physical dose distribution is attractive for sinonasal and skull base tumors because it can spare uninvolved contralateral structures more effectively than photons in many treatment scenarios. For ONB, reducing dose to the optic nerves, retina, temporal lobes, and hippocampi carries theoretical benefits for vision preservation, neurocognition, and secondary malignancy risk — outcomes particularly important in younger patients, who form a significant fraction of ONB cases.
Clinical caveats: Translating dosimetric advantages into meaningful clinical benefit requires demonstrating reduced rates of late complications or improved patient-centered outcomes without compromising tumor control. PBRT introduces distinct uncertainties: range uncertainty, sensitivity to tissue heterogeneity and setup variations, and higher relative cost and limited availability. Dosimetric planning differences, fractionation schemes, and institutional expertise may influence outcomes. The present study does not provide detailed dosimetric comparisons or long-term functional outcome measures (eg, formal vision testing, neurocognitive assessments, patient-reported quality of life), limiting mechanistic inference between dosimetry and clinical outcomes.
Strengths of the study
– Multicenter nature and inclusion of major tertiary skull base centers increase generalizability within high-volume academic settings.
– Propensity score matching on key baseline prognostic factors (age, modified Kadish stage, Hyams grade) was used to reduce measurable confounding between treatment groups.
– Long follow-up window adequate to capture late recurrences important in ONB.
Limitations and sources of uncertainty
– Small sample size: only 54 matched patients (18 PBRT), yielding wide confidence intervals and low statistical power to detect moderate differences in outcomes.
– Potential residual confounding: matching addressed some prognostic variables, but unmeasured confounders (extent of surgery, margin status, nodal disease, use of chemotherapy, performance status, and year of treatment) could bias comparisons.
– Heterogeneity in treatment era (2005–2021), evolving IMRT and PBRT planning/technology, surgical approaches, and supportive care practices may affect outcomes.
– Lack of detailed dosimetric data and functional long-term outcome measures limits assessment of clinically relevant benefits from organ sparing (eg, vision, cognition).
– Toxicity reporting had incomplete denominators (reported as 8 of 40 for overall RTAE), suggesting missing or variably captured toxicity data across centers.
Clinical implications
For clinicians counseling patients with ONB, the study provides important real-world comparative data but does not change practice definitively. Key practical points:
- IMRT remains an appropriate and effective standard adjuvant radiation modality for ONB with established local control and toxicity profiles.
- PBRT can be considered in selected patients when dosimetric planning demonstrates meaningful sparing of critical structures and in contexts where late toxicity avoidance is prioritized (eg, younger patients, preexisting optic or cognitive risks), but expectations should be tempered by the lack of high-quality comparative outcome data.
- Shared decision-making should incorporate patient values (eg, prioritizing reduction of late toxicities), institutional experience with PBRT, logistical considerations, and potential differences in cost and access.
Research and trial design recommendations
Because randomized trials in rare cancers are challenging, the authors’ dataset is a valuable step toward informing future studies. For an adequately powered comparative study, the field should consider:
- Prospective multicenter registry or randomized phase II/III trial with centralized review of pathology, staging, surgical margins, and radiation plans.
- Primary endpoints that combine disease control and clinically meaningful functional outcomes (eg, preservation of vision, neurocognitive function, patient-reported quality of life) rather than surrogate dosimetric endpoints alone.
- Mandatory collection of comprehensive dosimetric data and standardized normal tissue dose constraints to correlate dose–volume metrics with late toxicity.
- Sample size planning informed by the observed event rates: given the imprecision here, several hundred patients would likely be required to detect moderate differences in long-term RFS or toxicity, arguing for international collaboration and registry-based randomized designs.
Funding and clinicaltrials.gov
The published report did not identify a specific external funding source in the presented abstracted data. No clinical trial registration was cited for this retrospective cohort study. Future prospective studies should prospectively register on clinicaltrials.gov and report funding sources transparently.
Conclusion
In this propensity-matched cohort of 54 patients with olfactory neuroblastoma treated across nine tertiary centers, no clear advantage of proton beam radiotherapy over IMRT was demonstrated for local control, recurrence-free survival, overall survival, or grade ≥2 radiotherapy toxicity. Small sample size and wide confidence intervals preclude definitive conclusions. The data are hypothesis-generating and useful for planning adequately powered prospective comparative studies or registries that include rigorous dosimetric, functional, and patient-reported outcome collection.
References
1. Tang A, Adida S, Donohue J, et al. Proton Beam vs Intensity-Modulated Radiotherapy in Olfactory Neuroblastoma. JAMA Otolaryngol Head Neck Surg. 2025 Oct 30:e253816. doi:10.1001/jamaoto.2025.3816. PMID: 41165699; PMCID: PMC12576614.
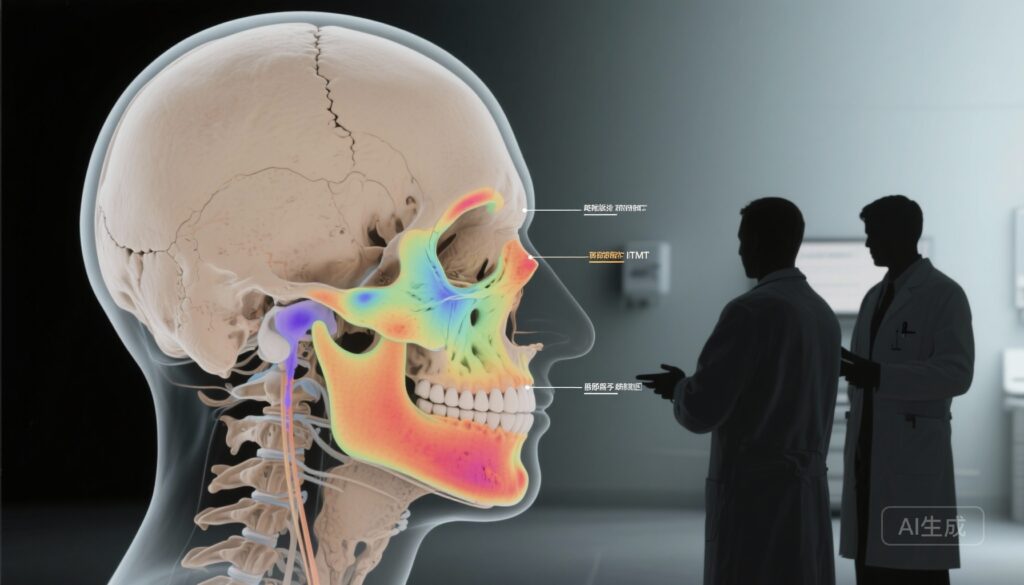
AI image prompt for article thumbnail
High-resolution clinical illustration of a head and skull base radiotherapy plan: overlay of anatomic MRI axial slice of the nasal cavity and anterior skull base with colored dose distributions for IMRT (plausible low-to-moderate spread) versus proton beam (sharper distal falloff), clinician silhouettes discussing a treatment plan in the foreground, neutral clinical color palette, photorealistic style