Highlights
– In a multicenter cohort of 3,980 patients with oral cavity squamous cell carcinoma (OCSCC), 39% received adjuvant therapy (AT) after surgery; 61% had surgery alone.
– Preoperative factors independently associated with receiving AT included younger age (<65 more likely than ≥65), higher comorbidity burden (CCI ≥4), prior head and neck cancer (less likely), specific subsites (maxillary alveolus, retromolar trigone), larger tumor dimension, higher clinical T and N stage, and poorer biopsy grade.
– Among patients receiving AT, poorly differentiated biopsy grade and advanced nodal stage predicted use of chemoradiation rather than radiotherapy alone. A predictive model using preoperative data achieved an AUC of 0.84.
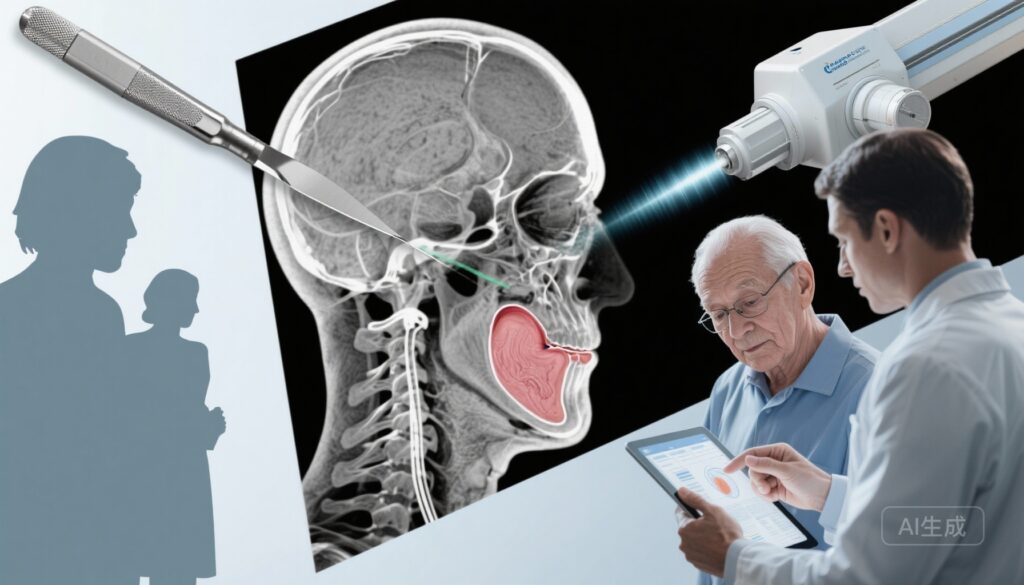
Background: disease context and unmet need
Primary surgical resection remains the cornerstone of therapy for resectable oral cavity squamous cell carcinoma (OCSCC). Decisions about adjuvant therapy (radiotherapy alone or concurrent chemoradiation) are typically driven by pathological features identified after surgery — notably positive surgical margins and extranodal extension (ENE) — which indicate high-risk disease and benefit from postoperative concurrent cisplatin-based chemoradiation. However, postoperative pathology is not available at the time of initial treatment planning. The ability to identify, preoperatively, patients who are likely to require AT could improve multidisciplinary planning, expedite referrals to radiation and medical oncology, reduce delays to adjuvant treatment, enhance patient counseling, and inform consent about expected morbidity and quality-of-life tradeoffs.
Study design and methods
The study by Dayan and colleagues (Canadian Head & Neck Collaborative Research Initiative) is a retrospective cohort analysis of consecutive patients with oral cavity cancer who underwent primary surgery across nine Canadian academic centers from January 2005 to December 2019. Data were abstracted for demographic variables (age, sex, smoking history, Charlson Comorbidity Index [CCI]), tumour characteristics available preoperatively (clinical T and N stage, biopsy grade, and tumor dimension), prior head and neck cancer history, and the eventual receipt of adjuvant therapy (none, postoperative radiotherapy [RT], or postoperative concurrent chemoradiation therapy [CRT]). The investigators examined associations between preoperative variables and: (1) receipt of AT versus surgery alone; (2) the type of AT (RT vs CRT); and (3) predictors of failure to receive AT among those who had strong pathologic indications for AT. Multivariable logistic regression models were used, and a predictive model for AT receipt was evaluated via area under the receiver operating characteristic curve (AUC). Data analysis was completed in March 2024.
Key findings
Overall cohort and outcomes
The cohort comprised 3,980 patients undergoing surgery for OCSCC. Mean age was 63 years (SD 13); 38% were female. Overall, 2,438 patients (61%) underwent surgery only, and 1,542 (39%) received adjuvant therapy. Strong pathologic indicators for AT (such as positive margins or extracapsular spread) were present in 1,907 patients (48%).
Preoperative predictors of receiving adjuvant therapy
On multivariable analysis, the following preoperative variables were independently associated with the odds of receiving AT after surgery:
- Age ≥65 years: associated with lower odds of receiving AT (OR 0.50; 95% CI, 0.38–0.64). In other words, older patients were less likely to receive postoperative RT/CRT.
- Charlson Comorbidity Index ≥4: higher odds of AT (OR 1.83; 95% CI, 1.26–2.65), suggesting clinicians may favor additional therapy in comorbid patients when tumor features are concerning.
- History of prior head and neck cancer: lower odds of AT (OR 0.40; 95% CI, 0.26–0.62), perhaps reflecting prior treatment exposures, prior irradiation, or different risk–benefit considerations.
- Tumour subsite: maxillary alveolus (OR 2.16; 95% CI, 1.11–4.22) and retromolar trigone (OR 1.85; 95% CI, 1.04–3.29) were associated with higher odds of AT, consistent with more locally aggressive behaviour or greater likelihood of high-risk pathologic features in these subsites.
- Tumour dimension (per cm increase): OR 1.35 (95% CI, 1.22–1.50), indicating larger tumors are more likely to require adjuvant therapy.
- Increasing clinical T and N stage: higher preoperative stage predicted higher likelihood of AT.
- Biopsy grade: poorly differentiated tumors on preoperative biopsy had increased odds of AT (OR 1.89; 95% CI, 1.25–2.84) compared with well- or moderately differentiated tumors.
Predictors of chemoradiation versus radiotherapy
Among those who received any AT, preoperative poorly differentiated grade (OR 2.40; 95% CI, 1.34–4.30) and more advanced nodal stage were associated with receipt of chemoradiation (CRT) rather than radiotherapy (RT) alone. This suggests that preoperative indicators of aggressive biology and nodal disease may foreshadow the need for intensification of adjuvant therapy.
Patients with strong pathologic indications who did not receive AT
Even among patients who had strong postoperative pathologic indicators for AT, certain preoperative factors were associated with not receiving recommended adjuvant treatment: older age, higher comorbidity burden, higher biopsy grade, advanced stage, and larger tumor dimension. These associations highlight complex clinical decision-making where chronological age, frailty, preexisting comorbidities, and perceived surgical risk may lead to omission of guideline-recommended postoperative therapy.
Model performance
The predictive model developed using preoperative variables showed good discrimination for predicting receipt of AT, with an AUC of 0.84 (95% CI, 0.82–0.86).
Clinical interpretation and implications
The findings indicate that a set of readily available preoperative clinical and tumor characteristics can meaningfully predict which patients are likely to require postoperative adjuvant therapy, and even which are likely to require CRT rather than RT alone. Key actionable implications include:
- Early multidisciplinary coordination: patients with larger tumors, higher clinical T/N stage, retromolar or maxillary alveolus subsites, and poorly differentiated biopsy grade can be triaged earlier to radiation and medical oncology consultation to streamline adjuvant planning and minimize delays between surgery and AT.
- Preoperative counseling and consent: surgeons can provide more accurate preoperative counselling about the likelihood of adjuvant therapy and its expected toxicities, aiding shared decision-making.
- Resource allocation and scheduling: predictive identification of likely AT candidates can help radiotherapy departments anticipate demand, reserve simulation slots, and schedule timely initiation of adjuvant therapy, which is associated with oncologic outcomes in head and neck cancer.
- Tailoring perioperative optimization: for patients predicted to require AT, early geriatric or comorbidity management and prehabilitation may improve tolerance and completion of adjuvant therapy.
Context with current evidence and guidelines
Adjuvant concurrent chemoradiation is recommended by contemporary guidelines (e.g., NCCN) for patients with high-risk pathologic features such as positive margins or extranodal extension; postoperative radiotherapy alone is favored for other high-risk but lower-intensity features. Landmark randomized trials demonstrated improved locoregional control and disease-free survival with the addition of cisplatin to postoperative radiotherapy in high-risk patients, establishing the standard for CRT in this setting. The present study complements these guidelines by identifying preoperative predictors that can anticipate which patients will ultimately be treated according to those postoperative criteria.
Strengths and limitations
Strengths of the study include a large, multicenter cohort across academic centers, a contemporary study period, and robust multivariable modeling with a high-performing predictive model.
Key limitations to consider:
- Retrospective observational design: subject to selection bias, unmeasured confounding, and practice variation across centers and over time.
- Heterogeneity in decision-making: the choice to omit adjuvant therapy can depend on nuanced clinical factors not fully captured in administrative or chart-review data (patient preference, frailty, prior radiation fields, functional status, social determinants, and multidisciplinary assessment).
- Pathology-driven decisions remain primary: while preoperative predictors are helpful, final decisions are necessarily contingent on postoperative pathologic findings (margins, extranodal extension, perineural invasion), which cannot be perfectly predicted from clinical data alone.
- Generalizability: practice patterns in Canadian academic centers may not fully reflect other health systems, community settings, or regions with different resource constraints.
Expert commentary and research priorities
From a clinical standpoint, this work reinforces the importance of preoperative risk stratification as part of a comprehensive head and neck oncology pathway. Multidisciplinary tumor boards should integrate preoperative predictors into scheduling and triage decisions to minimize time-to-adjuvant treatment — a known determinant of outcomes in head and neck cancer. Future prospective efforts should validate predictive models in external cohorts, evaluate integration with advanced imaging and molecular markers (eg, HPV status for oropharyngeal disease—less relevant to oral cavity), and determine whether preoperative prediction followed by expedited multidisciplinary interventions actually reduces time to AT and improves survival or functional outcomes.
Conclusion
Dayan et al. demonstrate that commonly available preoperative clinical and tumor features can predict the likelihood and intensity of adjuvant therapy following surgery for oral cavity squamous cell carcinoma. A predictive model with strong discriminatory performance (AUC 0.84) suggests these variables could be used in routine preoperative workflows to inform counseling, expedite multidisciplinary referrals, optimize resource planning, and potentially reduce delays to adjuvant therapy. Prospective validation and implementation research are needed to determine whether using such models improves timeliness of care and oncologic outcomes.
Funding and clinicaltrials.gov
The primary article reports funding and disclosures as listed in the JAMA Otolaryngology—Head & Neck Surgery publication. This was an investigator-initiated, multicenter retrospective cohort study; no clinicaltrials.gov registration applies to retrospective observational analyses.
Selected references
1. Dayan GS, Bahig H, Colivas J, et al. Preoperative Clinical and Tumor Factors Associated With Adjuvant Therapy for Oral Cavity Cancer. JAMA Otolaryngol Head Neck Surg. 2025;151(5):466–475. doi:10.1001/jamaoto.2024.5250.
2. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Head and Neck Cancers. Version current at time of writing (2024).
3. Cooper JS, Pajak TF, Forastiere AA, et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350(19):1937–1944.
4. Bernier J, Cooper JS, Pajak TF, et al. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation and chemotherapy trials of the EORTC and RTOG. Head Neck. 2005;27(10):843–850.
5. Amin MB, Edge SB, Greene FL, et al., editors. AJCC Cancer Staging Manual. 8th ed. Springer; 2017.