Background
Imagine this: Jane, a 52-year-old schoolteacher, sits across from her doctor after her annual checkup. Her blood pressure is creeping up, her cholesterol is borderline high, and she has gained 15 pounds over the last decade. Jane’s doctor discusses two paths. One involves a prescription for antihypertensive medication and statins. The other? A recommendation to overhaul her diet, start a walking routine, and manage her stress. Jane wonders: Can changing her plate truly replace her pills?
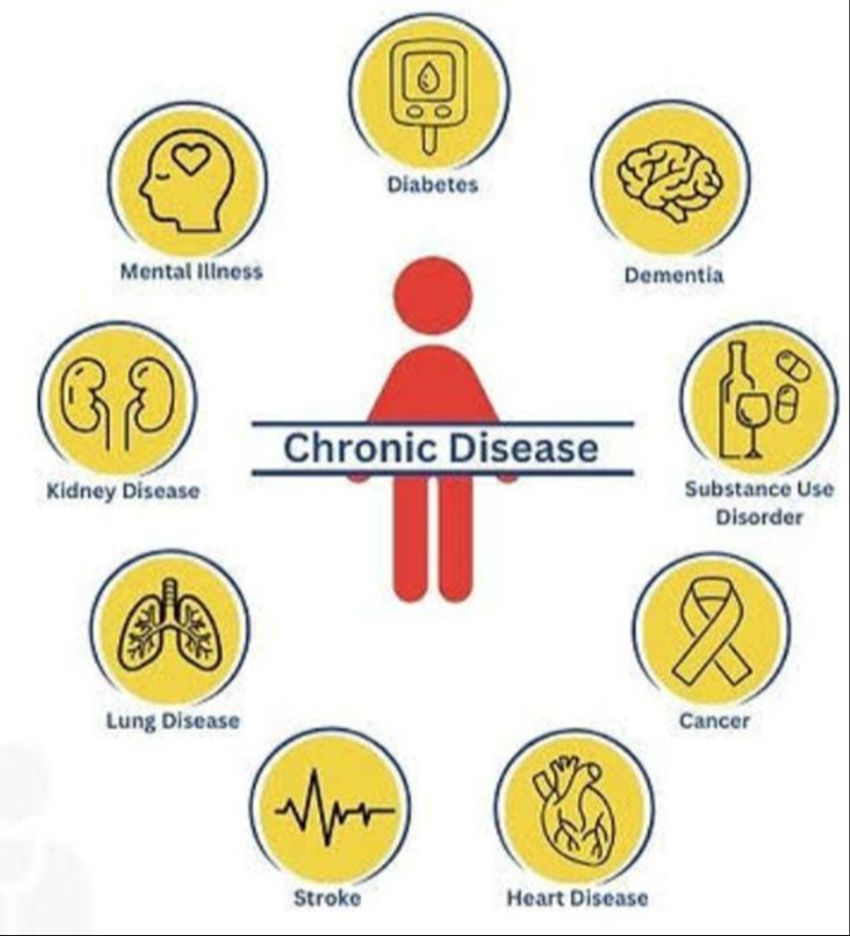
Chronic diseases—conditions like type 2 diabetes, hypertension, heart disease, and some forms of cancer—are the leading cause of death and disability worldwide. Traditionally, modern medicine has leaned heavily on pharmaceuticals to manage these conditions. But a growing movement in healthcare, known as lifestyle medicine, argues that what we eat, how we move, and our daily habits may be just as crucial—if not more so—than any pill.

Scientific and Clinical Evidence: What the Data Tell Us
Lifestyle medicine is not about shunning all medications. Instead, it focuses on evidence-based lifestyle interventions—such as nutrition, physical activity, sleep, stress management, social connection, and avoidance of risky substances—to prevent, treat, and even reverse chronic conditions.
In the past several decades, large-scale studies have demonstrated the profound impact of lifestyle on health outcomes:
– The Diabetes Prevention Program (DPP), a landmark U.S. trial, found that intensive lifestyle modification (diet, exercise, and modest weight loss) reduced the incidence of type 2 diabetes by 58%—outperforming the drug metformin, which reduced risk by 31%.
– The Ornish Lifestyle Medicine Program, which includes plant-based nutrition, stress management, exercise, and social support, has been shown to halt or even reverse coronary artery disease in select patients, as demonstrated by improvements in blood flow and reduction of arterial plaque on imaging studies.
– Meta-analyses confirm that dietary patterns such as the Mediterranean diet, rich in fruits, vegetables, whole grains, and healthy fats, significantly reduce the risk of cardiovascular disease, stroke, and certain cancers.
– Regular exercise, even brisk walking, lowers blood pressure and improves glycemic control in people with hypertension and diabetes, sometimes allowing for dose reduction or discontinuation of medications under professional supervision.
But is lifestyle medicine a “cure”? The answer is nuanced. For some individuals, intensive lifestyle change can lead to remission of disease. In others, it may reduce medication needs, improve quality of life, and prevent complications. Most clinicians agree: Lifestyle change is foundational, but not always a replacement for pharmaceuticals, especially in advanced or high-risk cases.
Misconceptions and Harmful Behaviors
Despite mounting evidence, several misconceptions persist:
– “If a little is good, more is better”: Extreme diets or exercise regimens can backfire, leading to nutritional deficiencies, injuries, or burnout.
– “I can stop my medication on my own if I feel better”: Abruptly stopping prescribed drugs can be dangerous. Medication adjustments should always be supervised by a healthcare professional.
– “Supplements can replace healthy eating”: No pill can mimic the complex benefits of a balanced, whole-foods diet.
– “Lifestyle medicine is only for prevention, not treatment”: In reality, it can play a therapeutic role in managing existing disease.
Social media often amplifies miracle cures and oversimplified solutions. This can lead to people trying unproven diets, rejecting necessary medications, or feeling shame if they can’t “heal themselves” through lifestyle alone.
Correct Health Practices and Practical Recommendations
So, what does the science-backed approach look like for someone like Jane?
1. **Nutrition**: Emphasize whole, minimally processed foods—vegetables, fruits, legumes, whole grains, nuts, and healthy oils. Limit red and processed meats, refined grains, and sugary beverages. Small, sustainable changes often work better than radical overhauls.
2. **Physical Activity**: Aim for at least 150 minutes of moderate-intensity activity (like brisk walking) per week, plus strength training twice weekly. Even short bouts of movement throughout the day count.
3. **Weight Management**: Modest weight loss (5-10% of body weight) can dramatically improve blood pressure, cholesterol, and blood sugar control in many people.
4. **Stress Management**: Practices like mindfulness, yoga, and deep breathing can lower stress hormones and inflammation, supporting heart and metabolic health.
5. **Sleep Hygiene**: Consistent, restorative sleep (7-9 hours) is essential for metabolic and cardiovascular health.
6. **Social Connection**: Meaningful relationships and support networks are linked to better health outcomes and lower mortality.
7. **Avoidance of Harmful Substances**: Avoid tobacco, limit alcohol, and minimize exposure to environmental toxins.
Crucially, lifestyle medicine works best when personalized and supported by a multidisciplinary team. Registered dietitians, exercise physiologists, therapists, and physicians can help tailor interventions to individual needs, medical histories, and cultural backgrounds.
Expert Insights and Commentary
Dr. Michael Evans, a family physician and leading voice in preventive medicine, explains: “We now understand that the root causes of most chronic diseases are behavioral and environmental. Medications are essential tools, but they’re not magic bullets. Empowering people to make sustainable lifestyle changes—while respecting the realities of modern life—can be transformative.”
He adds, “The real magic happens when patients feel supported, not judged. Small changes, done consistently, add up over time.”
Jane’s story is not unique. In recent years, healthcare systems have begun to integrate lifestyle medicine into standard care. Group visits, health coaching, and community-based programs are gaining ground. Employers and insurers are starting to recognize the cost savings of prevention and reversal, not just disease management.
Conclusion
Can lifestyle medicine “cure” chronic conditions? For some, it can lead to remission or reversal. For most, it’s an essential partner to medical therapy, improving outcomes and reducing medication needs. The best results come from a balanced approach: using pharmaceuticals wisely, while investing in the power of daily choices. Pills and plates are not rivals—they’re partners in modern healthcare.
Jane, after working closely with her healthcare team and making gradual lifestyle changes, found her blood pressure and cholesterol returning to healthy levels. Her doctor reduced her medication doses, but more importantly, Jane felt empowered—not just by a prescription, but by the knowledge and skills to care for herself.
References
1. Knowler WC, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393-403.
2. Ornish D, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280(23):2001-7.
3. Estruch R, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279-90.
4. American College of Lifestyle Medicine. What is Lifestyle Medicine? https://www.lifestylemedicine.org
5. American Heart Association. Life’s Essential 8. https://www.heart.org/en/healthy-living/healthy-lifestyle/lifes-essential-8