Highlights
- Oveporexton (TAK-861), an oral orexin receptor 2–selective agonist, significantly improved wakefulness and reduced cataplexy in patients with narcolepsy type 1.
- Significant improvements were observed on both the Maintenance of Wakefulness Test (MWT) and Epworth Sleepiness Scale (ESS) at 8 weeks versus placebo.
- The most frequent adverse events were insomnia, urinary urgency, and urinary frequency, with no hepatotoxicity reported.
- This phase 2 trial establishes clinical proof-of-concept for direct orexin receptor 2 agonism in narcolepsy type 1.
Clinical Background and Disease Burden
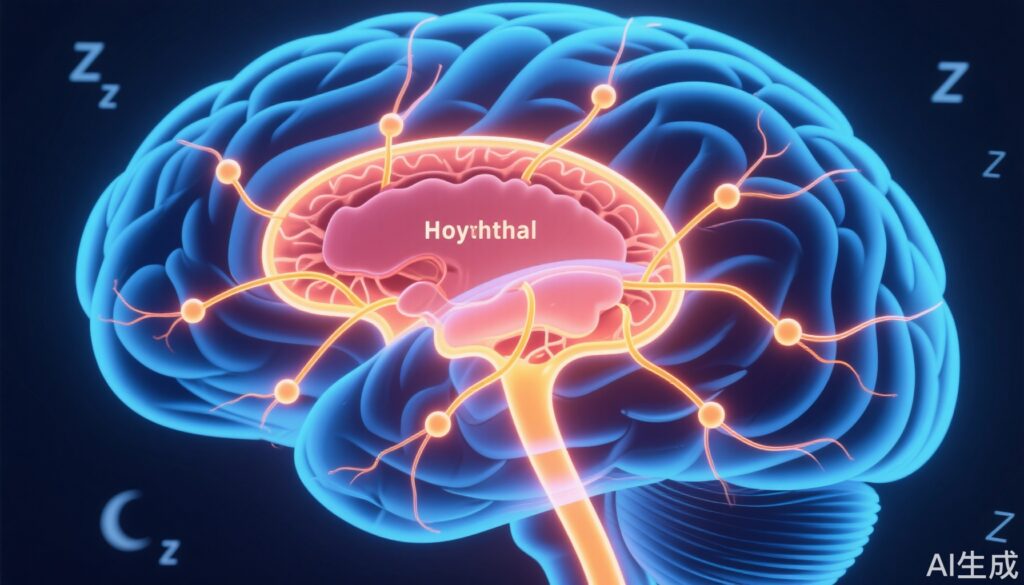
Narcolepsy type 1 is a chronic neurological disorder characterized by excessive daytime sleepiness, cataplexy (sudden muscle weakness triggered by emotions), sleep fragmentation, and other REM-sleep phenomena. The disease is caused by loss of hypothalamic neurons that produce orexin (hypocretin), a neuropeptide critical for stabilizing wakefulness. The resulting orexin deficiency leads to severe impairment in patients’ quality of life, social functioning, and vocational outcomes. Standard therapies, including stimulants and anticataplectics, provide symptomatic relief but do not address the underlying orexin deficit. An effective, disease-targeted therapy remains an unmet medical need.
Research Methodology
This multicenter, phase 2, randomized, placebo-controlled trial (TAK-861-2001; NCT05687903), evaluated the safety and efficacy of oveporexton, an oral orexin receptor 2–selective agonist, in adults with narcolepsy type 1. A total of 112 participants were randomized to receive once- or twice-daily oveporexton (0.5 mg twice daily, 2 mg twice daily, 2 mg followed by 5 mg daily, or 7 mg once daily) or placebo for 8 weeks. The primary endpoint was the mean change from baseline to week 8 in average sleep latency on the Maintenance of Wakefulness Test (MWT), a standard objective measure of the ability to remain awake. Secondary endpoints included the change in Epworth Sleepiness Scale (ESS) total score, weekly cataplexy rate at week 8, and adverse event monitoring.
Key Findings
Oveporexton demonstrated robust improvements across all efficacy endpoints compared to placebo:
- Mean changes in MWT sleep latency (in minutes) from baseline to week 8 were 12.5 (0.5 mg BID), 23.5 (2 mg BID), 25.4 (2 mg→5 mg QD), 15.0 (7 mg QD), versus −1.2 for placebo (adjusted P≤0.001 for all oveporexton arms vs. placebo). These values reflect a clinically meaningful restoration of wakefulness (normal MWT ≥20 minutes).
- ESS total scores decreased by −8.9, −13.8, −12.8, −11.3, and −2.5 points, respectively (adjusted P≤0.004 for all oveporexton arms vs. placebo), indicating substantial reductions in subjective daytime sleepiness (normal ESS ≤10).
- Weekly cataplexy rates at week 8 were 4.24, 3.14, 2.48, 5.89, and 8.76, respectively, with statistically significant reductions for the 2 mg BID and 2 mg→5 mg QD regimens (adjusted P<0.05 vs. placebo).
- Adverse events were more frequent in oveporexton groups, notably insomnia (48% of participants; mostly resolving within 1 week), urinary urgency (33%), and urinary frequency (32%). No cases of hepatotoxicity were observed.
Mechanistic Insights and Biological Plausibility
The pathophysiology of narcolepsy type 1 centers on near-complete loss of orexin-producing neurons, leading to deficient signaling through orexin receptors, especially orexin receptor 2 (OX2R). Oveporexton is a selective OX2R agonist designed to mimic endogenous orexin activity, directly addressing the core neurochemical deficit. The rapid and sustained improvements in wakefulness and cataplexy rates seen in this study provide clinical validation for OX2R agonism as a rational, disease-modifying approach.
Expert Commentary
Leading narcolepsy experts, including Dr. Emmanuel Mignot (a co-author and pioneer in narcolepsy research), have previously highlighted the potential of orexin-based therapeutics to fundamentally change disease management, as they target the underlying etiology rather than downstream symptoms. The present results align with this paradigm shift, suggesting that oveporexton could represent a first-in-class therapy for narcolepsy type 1.
Controversies and Limitations
While the trial’s findings are promising, several limitations merit consideration:
- Short duration: The 8-week treatment period precludes assessment of long-term efficacy, safety, and rare adverse events.
- Sample size: The study enrolled a modest number of participants (n=112), limiting power for subgroup analyses and detection of uncommon safety signals.
- Dose optimization: Although multiple regimens were tested, the optimal long-term dosing strategy remains to be established.
- Generalizability: The study focused exclusively on narcolepsy type 1; efficacy in narcolepsy type 2 or other hypersomnolence disorders is unknown.
Conclusion
This phase 2 randomized trial provides robust evidence that oveporexton, an oral orexin receptor 2–selective agonist, significantly improves wakefulness, reduces excessive daytime sleepiness, and mitigates cataplexy in narcolepsy type 1 patients over 8 weeks. The safety profile is favorable, with no hepatotoxicity observed. These results herald a potential paradigm shift toward disease-targeted therapy in narcolepsy. Ongoing and future phase 3 trials will be critical to confirm long-term efficacy and safety, optimize dosing, and define the role of oveporexton in clinical practice.
References
Dauvilliers Y, Plazzi G, Mignot E, Lammers GJ, Del Río Villegas R, Khatami R, Taniguchi M, Abraham A, Hang Y, Kadali H, Lamberton M, Sheikh S, Stukalin E, Neuwirth R, Swick TJ, Tanaka S, von Hehn C, von Rosenstiel P, Wang H, Cai A, Naylor M, Olsson T. Oveporexton, an Oral Orexin Receptor 2-Selective Agonist, in Narcolepsy Type 1. N Engl J Med. 2025 May 15;392(19):1905-1916. doi: 10.1056/NEJMoa2405847. PMID: 40367374.