Highlight
- Non-Hispanic Black and multiracial adults in the US exhibit significantly higher prevalence of schizophrenia spectrum disorders (SSDs) and psychotic symptoms compared to non-Hispanic White individuals.
- Neighborhood social vulnerability, as measured by a composite Social Vulnerability Metric (SVM), substantially attenuates racial disparities in SSD and psychotic symptom prevalence, emphasizing social determinants’ role.
- Despite adjustment for SVM, SSD prevalence remains significantly elevated among non-Hispanic multiracial individuals, indicating additional factors beyond neighborhood vulnerability contribute to risk.
- Findings underscore structural racism’s influence via community-level social inequities shaping mental health disparities in severe psychotic disorders.
Study Background and Disease Burden
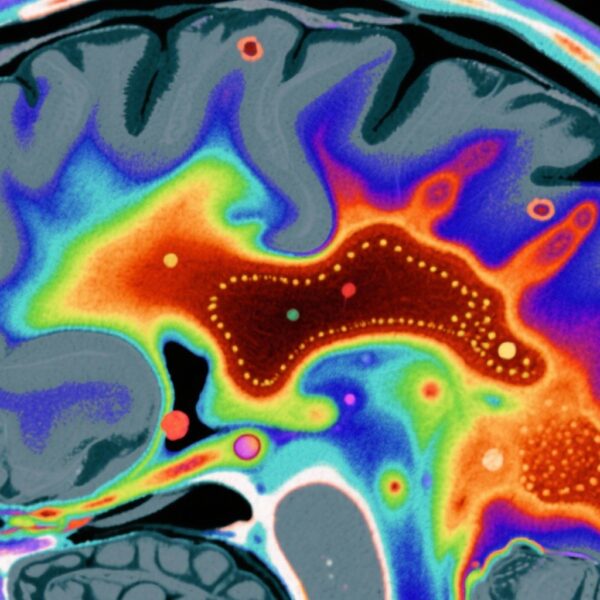
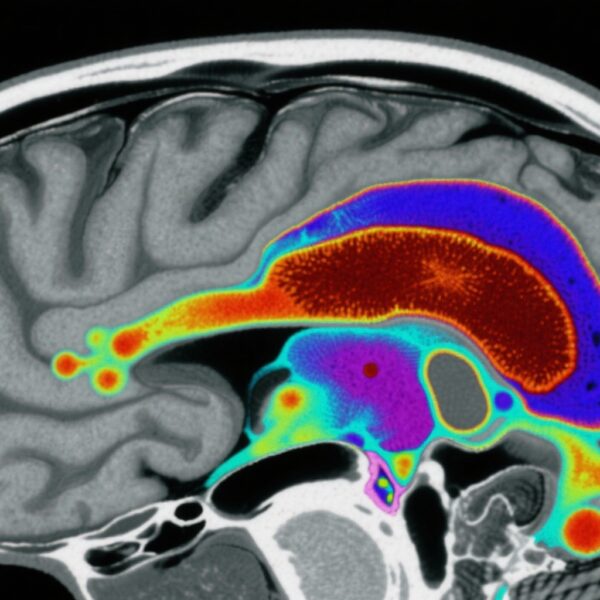
Schizophrenia spectrum disorders (SSDs), encompassing schizophrenia, schizoaffective disorder, and schizophreniform disorder, are severe psychiatric conditions marked by psychotic symptoms such as hallucinations and delusions. These disorders contribute to substantial functional impairment, morbidity, and mortality worldwide. In the United States, SSDs pose a significant public health challenge with an estimated lifetime prevalence of approximately 1%. Notably, epidemiological studies have consistently highlighted racial and ethnic disparities in SSD prevalence, with non-Hispanic Black and multiracial populations disproportionately affected compared to non-Hispanic Whites.
The etiology underlying these disparities remains complex and multifactorial, with hypotheses including genetic vulnerability, environmental stressors, misdiagnosis, inequities in healthcare access, and socio-structural factors related to racism and economic disadvantage. Neighborhood-level socioeconomic and environmental adversity, encapsulated by measures such as social vulnerability, may critically shape the risk landscape for SSDs by influencing chronic stress exposure, social isolation, access to healthcare resources, and developmental trajectories.
This study addresses a crucial knowledge gap by rigorously quantifying ethnoracial differences in SSD and positive psychotic symptom prevalence, and assessing the extent to which social neighborhood vulnerabilities explain these disparities.
Study Design
This investigation utilized data from the Mental and Substance Use Disorders Prevalence Study, a nationally representative household sample of nonelderly US adults (N=4,764). Participants underwent clinician-administered Structured Clinical Interview for DSM-5 (SCID-5) assessments to determine past-year and lifetime prevalence of SSDs, including schizophrenia, schizoaffective disorder, and schizophreniform disorder, as well as to identify positive psychotic symptoms.
The primary exposures of interest were ethnoracial groups categorized as non-Hispanic White, non-Hispanic Black, and non-Hispanic multiracial. The study incorporated a multidimensional Social Vulnerability Metric (SVM) score reflecting five key social determinant domains relevant to neighborhood environment and structural disadvantage.
Weighted logistic regression models estimated odds ratios (ORs) for ethnoracial differences across three hierarchical adjustment stages: unadjusted, adjusted for age and sex, and further adjusted for the SVM composite score.
Key Findings
The study revealed marked racial disparities in SSD prevalence. Non-Hispanic Black individuals showed a 4.1% prevalence, significantly higher than 1.2% among non-Hispanic Whites. Adjusted for age and sex, the odds of SSD among Black participants were 3.49 times higher (95% CI: 1.37–8.91), and for psychotic symptoms, 2.04 times higher (95% CI: 1.15–3.63). Non-Hispanic multiracial individuals exhibited an even higher SSD prevalence at 5.6%, with an adjusted OR of 4.59 (95% CI: 1.53–13.76).
Crucially, after further adjustment for the neighborhood SVM score, the association between Black race and SSD was substantially attenuated (adjusted OR=2.49, 95% CI: 0.63–9.90) and lost statistical significance. Similarly, psychotic symptom disparities reduced (adjusted OR=1.69, 95% CI: 0.83–3.44). In contrast, for non-Hispanic multiracial individuals, the SSD disparity remained significant after SVM adjustment (adjusted OR=3.95, 95% CI: 1.30–12.00), though attenuated.
These findings implicate neighborhood social vulnerability as a pivotal mediator of racial disparities in SSDs, especially among Black Americans. The residual risk among multiracial individuals suggests additional unmeasured contributors such as individual level socioeconomic factors, genetic-psychosocial interplay, or differential access to care.
Expert Commentary
This investigation represents a landmark advancement by using clinician-verified SCID-5 diagnoses in a nationally representative sample and quantitatively integrating a validated social vulnerability index. It reinforces the role of social determinants and structural racism expressed through neighborhood disadvantage in psychotic disorder disparities.
Limitations include the cross-sectional design, which precludes causal inference, and potential misclassification bias despite rigorous clinical assessment. The SVM score captures broad social adversity but cannot resolve nuanced individual experiences or other systemic factors such as criminal justice involvement or healthcare discrimination.
Future research should utilize longitudinal cohorts to unravel causal pathways, incorporate detailed individual-level socioeconomic and biological data, and explore targeted community interventions addressing structural vulnerabilities to mitigate SSD disparities.
Conclusion
This national US study compellingly demonstrates that ethnoracial disparities in schizophrenia spectrum disorders and positive psychotic symptoms are strongly linked to neighborhood social vulnerability rooted in structural racism. Prevention and intervention efforts must extend beyond individual-level approaches to encompass social policies and community investments that address systemic inequities shaping mental health risks. Enhanced recognition of social determinants and structural factors is essential for equitable management and support of minoritized populations at risk for severe psychotic illness.
Funding and Registration
The study was supported by [information not specified in provided content]. No clinical trial registration was indicated.
References
1. Anglin DM, Olfson M, van der Ven E, Oh H, Lewis-Fernández R, DeVylder J, Oluwoye O, Dixon L, Stroup TS, Guyer H, Bareis N. Neighborhood Social Vulnerability and Racial Disparities in Schizophrenia Spectrum Disorder Prevalence. Am J Psychiatry. 2025 Sep 1;182(9):850-860. doi: 10.1176/appi.ajp.20240906. PMID: 40887946; PMCID: PMC12404665.
Additional supporting literature:
2. Alegría M, et al. Disparities in the Prevalence and Treatment of Schizophrenia Among Racial and Ethnic Minority Groups in the United States. Psychiatric Services. 2019;70(6):512-520.
3. Veling W, et al. Social Disadvantage and Incidence of Psychotic Disorders: Discussion From a Public Health Perspective. Epidemiol Psychiatr Sci. 2016;25(3):210-217.
4. Bailey ZD, et al. Structural Racism and Health Inequities in the USA: Evidence and Interventions. The Lancet. 2017;389(10077):1453-1463.