Highlight
– In children and adolescents with obesity, greater lower limb muscular strength is associated with markedly reduced odds of metabolic syndrome (MetS).
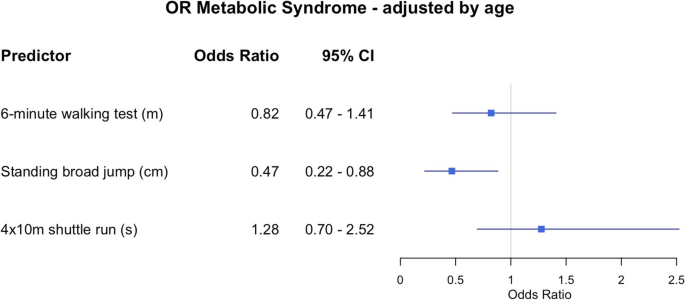
– Every 24-cm increase in standing broad jump (SBJ) performance correlates with a 53% reduction in the odds of MetS (OR 0.47; 95% CI: 0.22–0.88).
– Cardiorespiratory fitness and speed-agility were not significantly linked to MetS risk.
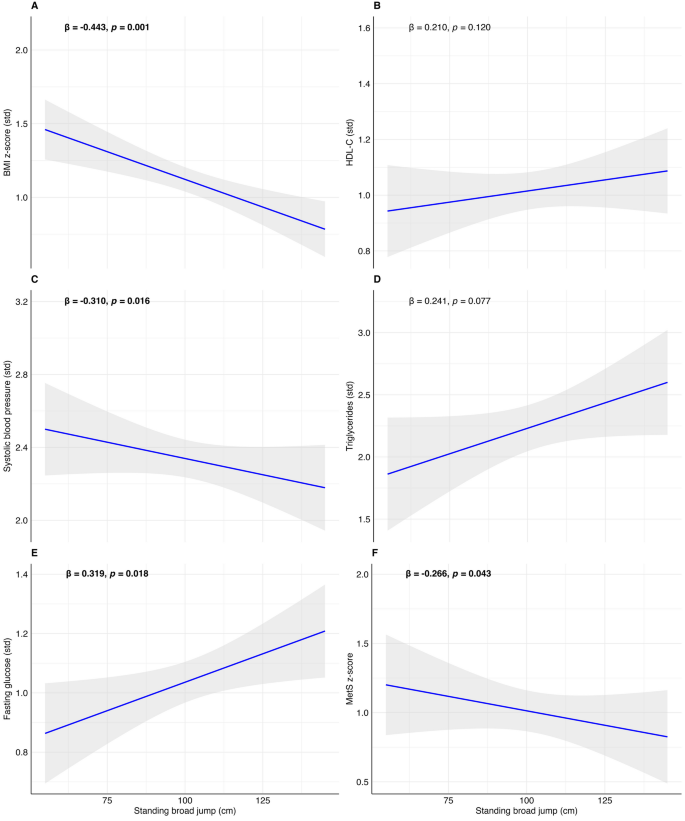
– Muscular strength showed inverse associations with BMI z-score and systolic blood pressure but a positive association with fasting glucose.
Background
Childhood obesity is a global epidemic, with prevalence rates rising sharply over the past decades. The associated burden includes increased risk for metabolic syndrome—a cluster of cardiometabolic abnormalities encompassing central obesity, hypertension, dyslipidaemia, and hyperglycaemia. Early-life MetS is a harbinger for type 2 diabetes and premature cardiovascular disease, making its prevention and early intervention a public health priority. While cardiorespiratory fitness is frequently championed for its protective metabolic effects, the independent role of muscular strength in paediatric metabolic health remains less explored in clinical settings.
Study Overview and Methodological Design
A cross-sectional study by Vandoni et al., conducted in a paediatric hospital in Milan, Italy, between March 2024 and February 2025, aimed to clarify the relationship between specific domains of physical fitness and metabolic risk in children with obesity. The investigators recruited 62 participants aged 6–17 years (mean age 11.4, 40.3% girls), all with a BMI z-score >2 SD, denoting significant obesity. The MetS risk score was calculated using validated formulas incorporating BMI z-score, systolic blood pressure, high-density lipoprotein cholesterol (HDL-C), triglycerides, and fasting glucose, with MetS defined as a score >0.75.
The formula to assess the MetS risk score is presented below:
- Boys
- MetS risk score = − 4.931 + 0.2804 * BMI z-score − 0.0257 * HDL-C + 0.0189 * Systolic blood pressure + 0.6240 * log(triglycerides) + 0.0140 * fasting glucose
- Girls
- MetS risk score = − 4.3757 + 0.4849 * BMI z-score − 0.0176 * HDL-C + 0.0257 * Systolic blood pressure + 0.3172 * log(triglycerides) + 0.0083 * fasting glucose
Physical fitness was objectively assessed using three measures: the 6-minute walk test (6MWT; cardiorespiratory fitness), standing broad jump (SBJ; lower limb muscular strength), and the 4 × 10-m shuttle run (speed-agility). The study adjusted for confounders including age and sex in its analyses.
Key Findings
Among the cohort, the prevalence of MetS was 64.5%. The most striking result was the strong inverse relationship between lower limb muscular strength (SBJ) and MetS risk. Each standard deviation (24 cm) increment in SBJ distance was associated with a 53% reduction in the odds of MetS (adjusted OR 0.47, 95% CI 0.22–0.88).
Fig. 1
Forest plot of adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for predictors of metabolic syndrome in children with obesity. Each row displays a specific predictor, with the square dot representing the adjusted for age odds ratio and the horizontal line extending from the dot indicating the 95% confidence interval. The plot includes a vertical reference line at an OR of 1.0, representing no effect. Predictors with confidence intervals that do not cross this line suggest a statistically significant association with metabolic syndrome. The numerical values of the odds ratio values and their CI are placed next to each predictor
Fig. 2
Associations between standing broad jump (cm) with BMI z-score (A), high-density lipoprotein (HDL-C, B), systolic blood pressure (C), triglycerides (D), fasting glucose (E), and metabolic syndrome risk score (MetS risk score, F) in children with obesity. Shading indicates the 95% confidence intervals of the associations. Bold beta and p-value indicate statistically significant associations (p < 0.05)
SBJ performance was also inversely correlated with BMI z-score (β = –0.443, p = .001) and systolic blood pressure (β = –0.304, p = .020), suggesting broader cardiovascular benefits. However, SBJ was positively associated with fasting glucose (β = 0.319, p = .018), a finding warranting further exploration. In contrast, neither cardiorespiratory fitness (6MWT) nor speed-agility (4 × 10-m run) showed significant associations with MetS risk. Notably, agility was positively related to BMI z-score (β = 0.331, p = .016), but not to other metabolic parameters.
Mechanistic Insights and Pathophysiological Context
The biological plausibility of these findings is underpinned by the emerging recognition of skeletal muscle as a critical regulator of metabolic health. Muscle tissue, particularly in the lower limbs, is a major site for insulin-mediated glucose uptake and triglyceride clearance. Enhanced muscle strength may reflect greater muscle mass and improved muscle quality, both of which are associated with higher metabolic flexibility and reduced adiposity-driven inflammation. Conversely, poor muscular fitness may perpetuate insulin resistance, lipid derangements, and hypertension, all core features of MetS. The positive association between muscular strength and fasting glucose in this cohort is unexpected and may represent an adaptive response to higher muscle mass or a limitation related to cross-sectional design and confounding factors.
Clinical Implications
For clinicians managing paediatric obesity, these data suggest that muscular strength assessments—such as the standing broad jump—should be considered alongside traditional anthropometric and cardiometabolic evaluations. Targeted interventions to improve muscle strength, possibly via resistance training or structured physical activity programs, could offer additive benefits for metabolic health beyond aerobic fitness alone. Integrating muscle-strengthening activities into paediatric obesity management may be particularly advantageous for children at highest risk for MetS.
Limitations and Controversies
Several limitations merit consideration. The study’s cross-sectional design precludes causal inferences. The sample size, while adequate for exploratory analyses, limits generalisability and the ability to stratify by pubertal status, sex, or ethnicity. The positive correlation between muscular strength and fasting glucose is counterintuitive and highlights the need for longitudinal research to clarify directionality. Additionally, physical fitness was assessed via field tests, which may be influenced by motivation, technique, and environmental factors. No intervention or control group was included. Finally, while the findings are compelling, they require replication in larger, multi-ethnic cohorts and with more precise measures of muscle mass and metabolic parameters.
Expert Commentary or Guideline Positioning
Current paediatric obesity guidelines, including those from the American Academy of Pediatrics and the Endocrine Society, emphasize comprehensive lifestyle interventions combining dietary, aerobic, and resistance training elements. The present study lends empirical support to the inclusion of muscle-strengthening activities as a core component of metabolic risk reduction strategies. As noted by the authors, early education on the value of daily physical activity and muscle integrity is paramount for establishing lifelong health trajectories.
Conclusion
This study adds to a growing body of evidence positioning muscular strength as a pivotal, modifiable determinant of metabolic syndrome risk in children and adolescents with obesity. While aerobic fitness remains important, muscular fitness—assessed simply by standing broad jump—may offer unique prognostic and therapeutic value. Future research should prioritise longitudinal and interventional designs to elucidate causality and refine paediatric exercise prescriptions. For now, the message is clear: building stronger muscles in youth may be a critical step in breaking the intergenerational cycle of cardiometabolic disease.
References
1. Vandoni M, Gatti A, Carnevale Pellino V, Marin L, Cavallo C, Rossi V, Lascialfari G, Zuccotti G, Calcaterra V. Exploring the link between metabolic syndrome risk and physical fitness in children with obesity: a cross-sectional study. Eur J Pediatr. 2025 Jul 24;184(8):497. doi: 10.1007/s00431-025-06339-7 IF: 2.6 Q1 . PMID: 40705115 IF: 2.6 Q1 ; PMCID: PMC12289717 IF: 2.6 Q1 .2. American Academy of Pediatrics. Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity. Pediatrics. 2023.3. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362-74.