Highlight
The FLAVOUR trial extended follow-up reveals no significant difference in major adverse outcomes between fractional flow reserve (FFR) and intravascular ultrasound (IVUS)-guided PCI in intermediate coronary stenosis over 6 years. FFR guidance leads to fewer total target vessel interventions, despite a higher incidence of late revascularization in initially deferred lesions.
This study informs clinical decision-making on optimal lesion assessment in intermediate coronary stenosis with implications for procedural strategy and long-term patient management.
Study Background and Disease Burden
Intermediate coronary artery stenoses, characterized by 40%-70% luminal narrowing, represent a clinical grey zone in cardiovascular intervention decision-making. These lesions pose challenges for determining the necessity and timing of percutaneous coronary intervention (PCI). Traditional angiography-based assessment has limitations in accurately identifying ischemia-producing lesions, leading to potential over- or undertreatment.
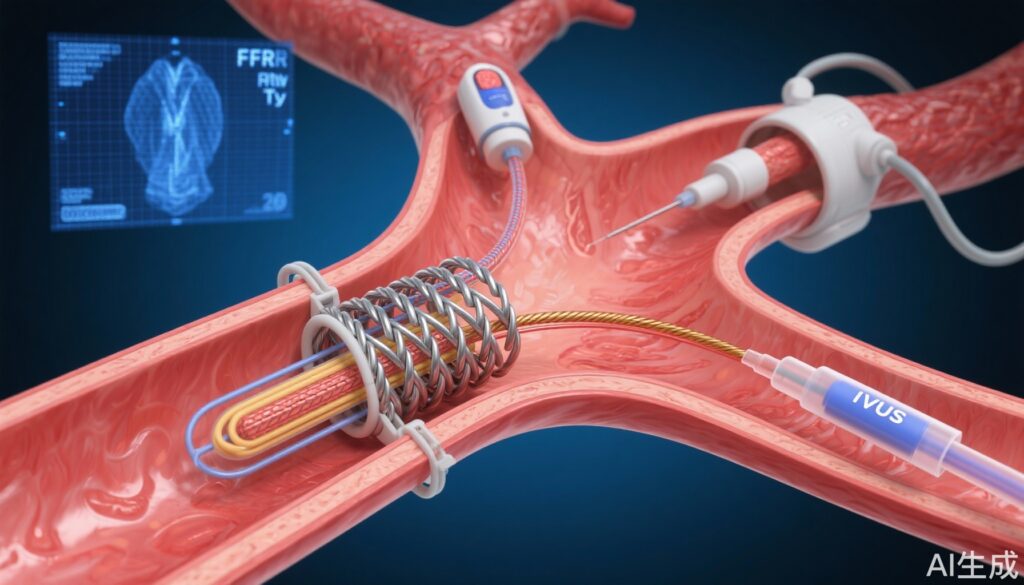
Fractional flow reserve (FFR) and intravascular ultrasound (IVUS) are two widely utilized modalities to guide PCI. FFR provides a physiological assessment of lesion significance by measuring pressure gradients during induced hyperemia, while IVUS offers high-resolution anatomical images including plaque burden and vessel size.
Despite existing data supporting both modalities, direct comparisons on long-term outcomes are scarce, particularly in intermediate stenoses. The FLAVOUR trial was designed to address this gap by evaluating clinical outcomes using these strategies across a large, multinational cohort.
Study Design
The FLAVOUR trial was a randomized, open-label, multinational study conducted across 18 sites in Korea and China. It enrolled patients aged 19 years or older with de novo intermediate coronary stenosis (40%-70%) and target vessel diameters ≥2.5 mm.
Patients were randomized 1:1 to either FFR-guided or IVUS-guided PCI strategies. In the FFR group, PCI was performed based on ischemic threshold criteria, typically FFR ≤0.80. In the IVUS arm, PCI decisions relied on morphological assessment parameters, including minimal lumen area and plaque characteristics.
The primary endpoint was a composite outcome of all-cause death, myocardial infarction, and any subsequent revascularization after the index procedure. Secondary endpoints comprised the individual components of the primary endpoint and per vessel analyses according to treatment intervention type.
Extended follow-up was prospectively conducted through September 2024, providing up to 7 years of outcome data, with a median of 6.3 years.
Key Findings
A total of 1,682 patients were enrolled and randomized: 838 to the FFR-guided group and 844 to the IVUS-guided group. The median follow-up duration was 6.3 years (interquartile range 5.6 to 6.9 years).
The primary composite endpoint occurred in 339 patients (22.0%) overall. Event rates were 23.1% in the FFR group and 20.9% in the IVUS group, with no statistically significant difference (hazard ratio [HR] 1.15; 95% confidence interval [CI] 0.93-1.42; P=0.208).
Revascularization following the index procedure was more frequent in the FFR group (14.9% vs 11.8%; HR 1.32; 95% CI 1.00-1.75; P=0.049), driven primarily by target vessel revascularization (9.6% vs 6.2%; HR 1.67; 95% CI 1.15-2.43; P=0.007).
Landmark analysis at 2 years demonstrated that the elevated revascularization rate in the FFR group was predominantly due to late (2-7 years) revascularizations in vessels where PCI was initially deferred based on FFR assessment.
Importantly, when considering both the initial PCI procedures and subsequent revascularizations, the overall rate of target vessel PCI was significantly lower in the FFR group compared to IVUS (38.8% vs 60.5%; P<0.001), reflecting a more conservative intervention approach guided by physiological criteria.
No significant differences in all-cause mortality or myocardial infarction rates were observed between the two groups during the extended follow-up period.
Expert Commentary
The FLAVOUR trial adds critical long-term evidence to the ongoing debate regarding intermediate coronary stenosis management. Its findings support the safety and efficacy of FFR guidance in deferring PCI safely in a substantial proportion of patients without increasing death or myocardial infarction. However, the higher incidence of late revascularization in initially deferred vessels suggests that some lesions deemed non-ischemic by FFR may progress or have under-recognized ischemic potential.
The significantly lower overall target vessel PCI rate with FFR guidance has implications for resource utilization, procedural risks, and patient burden. Conversely, IVUS guidance tends to lead to more frequent initial interventions, potentially addressing more anatomical lesion features but without evident long-term clinical superiority.
Notably, the multinational setting and large sample size strengthen the generalizability of the results, although regional cardiovascular risk factor variations and practice patterns should be factored into interpretation.
Potential limitations include the open-label design and adherence variability to PCI thresholds. Future studies integrating multi-modality imaging and physiology may further refine patient-specific strategies.
Conclusion
The extended 6.3-year follow-up of the FLAVOUR trial demonstrates that FFR- and IVUS-guided PCI strategies in intermediate coronary stenosis yield comparable patient-oriented composite outcomes. FFR guidance enables deferral of PCI in many lesions, resulting in fewer total target vessel interventions without compromising mortality or myocardial infarction risk.
Clinicians should consider FFR-guided assessment as a safe and cost-effective approach for managing intermediate stenosis, while being vigilant about the potential need for late revascularization in initially deferred lesions. Integration of physiological and anatomical data, combined with longer-term surveillance, may optimize individualized treatment approaches.
References
Yang S, Hu X, Zhang J, Jiang J, Hahn JY, Doh JH, Lee BK, Kim W, Huang J, Jiang F, Zhou H, Chen P, Tang L, Jiang W, Chen H, Chen X, He W, Ahn SG, Tahk SJ, Kim U, Hwang D, Kang J, Ki YJ, Shin ES, Nam CW, Wang J, Koo BK; FLAVOUR Investigators. Long-Term Outcomes After Fractional Flow Reserve vs Intravascular Ultrasound to Guide PCI: The FLAVOUR Trial Extended Follow-Up. J Am Coll Cardiol. 2025 Aug 26;86(8):593-606. doi: 10.1016/j.jacc.2025.06.042. PMID: 40835367.