Highlight
- Transcatheter aortic valve implantation (TAVI) shows early superiority over surgical aortic valve replacement (SAVR) in preventing death or stroke, especially in high-risk patients.
- This benefit attenuates over the long term, with no statistically significant difference observed at 5-year follow-up across low, intermediate, and high-risk groups.
- Risk profile strongly influences event rates, with high-risk patients experiencing greater absolute benefits from TAVI over time.
Study Background
Aortic valve disease, particularly aortic stenosis, represents a substantial cause of morbidity and mortality globally. Surgical aortic valve replacement (SAVR) has been the standard of care for severe symptomatic cases for decades. Recently, transcatheter aortic valve implantation (TAVI) has emerged as a less invasive alternative, initially reserved for patients at prohibitive or high surgical risk. Indications for TAVI have since expanded to intermediate and low-risk populations, spurred by favorable short-term outcomes. However, long-term data on device durability, comparative effectiveness, and safety remain limited. This meta-analysis specifically addresses these uncertainties by comparing TAVI and SAVR with a 5-year perspective across different surgical risk profiles.
Study Design
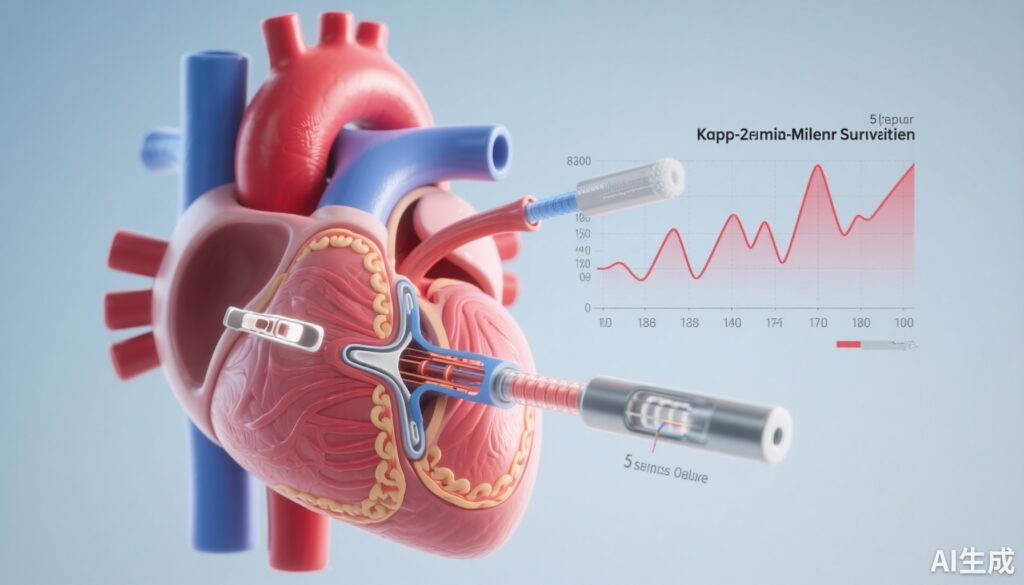
This analysis synthesized evidence from eight randomized controlled trials (RCTs) enrolling 9,811 participants randomized to undergo either TAVI or SAVR. Eligible studies included head-to-head comparisons with a minimum follow-up extending to five years. The primary endpoint was a composite of all-cause mortality or stroke occurring during follow-up. Risk stratification was performed categorizing patients into high, intermediate, and low surgical risk based on baseline clinical characteristics.
Time-to-event data were reconstructed from published Kaplan-Meier survival curves to calculate hazard ratios (HRs) and differences in restricted mean survival time (RMST), providing nuanced insight into how treatment effects evolve over the duration of follow-up.
Key Findings
Event rates for death or stroke progressively increased with higher baseline risk irrespective of treatment modality. Transcatheter therapy demonstrated a time-variant effect characterized by an early survival and stroke-free advantage, particularly in high-risk patients.
Specifically, at four years, TAVI was associated with an additional 0.77 months free of the composite endpoint compared to SAVR, driven primarily by outcomes in the high-risk subgroup. This early benefit progressively attenuated by five years. In the high-risk group, the trend toward benefit persisted with an RMST difference of 2.39 months favoring TAVI over SAVR, though this just missed conventional statistical significance (95% CI: -0.23 to 5.02; p=0.07).
For intermediate and low-risk groups, benefits of TAVI followed a quadratic association — initial incremental improvements were observed but diminished over time, showing minimal differences at 60 months post-procedure (low-risk RMST difference 0.86 months, 95% CI: -0.11 to 1.84, p=0.09; intermediate-risk RMST difference 0.45 months, 95% CI: -0.66 to 1.56, p=0.42).
Collectively, at the 5-year endpoint, no statistically significant difference was observed between TAVI and SAVR across all risk profiles for the composite outcome of death or stroke.
Expert Commentary
This comprehensive meta-analysis offers valuable insight into the long-term comparative effectiveness of TAVI versus SAVR, highlighting the dynamic nature of risk-benefit balance influenced by baseline surgical risk. Early procedural advantages of TAVI, such as less invasiveness leading to lower perioperative mortality and stroke rates, appear to diminish as longer-term factors such as valve durability, structural valve deterioration, and late complications play a greater role.
Recent guidelines cautiously endorse TAVI as an equivalent option in intermediate and low-risk populations, largely supported by shorter-term data. However, findings from this meta-analysis underscore the necessity of prolonged surveillance beyond five years, particularly when considering expanding TAVI indications in younger, low-risk patients with longer life expectancy.
Limitations include reconstructed time-to-event data extracted from Kaplan-Meier curves rather than raw individual patient data, which may introduce imprecision. Additionally, heterogeneity in device types, procedural techniques, and patient selection over the timeline of the included trials should be considered when extrapolating results. Further dedicated research is required to define optimal patient selection and to monitor long-term valve performance.
Conclusion
In summary, while TAVI provides a clear early benefit over SAVR regarding all-cause mortality or stroke—especially in high-risk patients—these advantages attenuate and are not statistically significant at five years. Risk stratification remains integral to procedural decision-making, and long-term follow-up will be essential to optimize management strategies for aortic valve disease as TAVI indications continue to broaden.
Funding and Clinical Trials Registration
Not reported in the meta-analysis source article. Individual trials included in the analysis may have varied funding and registration details.
References
Barili F, Pollari F, Marin-Cuartas M, Anselmi A, de la Cuesta M, Brophy JM, Boden WE, De Caterina R, Dayan V, Roda JR, Uva MS, Almeida RMS, Tomasi J, Verhoye JP, Musumeci F, Mandrola J, Kaul S, Papatheodorou S, Parolari A; Integritty. Time-to-event analysis of the long-term outcome in trials comparing transcatheter and surgical aortic valve implantation: A meta-analysis. Int J Cardiol. 2025 Nov 1;438:133524. doi: 10.1016/j.ijcard.2025.133524. Epub 2025 Jun 24. PMID: 40571128.