Introduction
Relapsed or refractory large B-cell lymphoma (LBCL) remains a clinical challenge where conventional therapies often yield suboptimal long-term outcomes. Despite advances, patients with primary refractory or early relapsed LBCL within 12 months after first-line therapy typically face poor prognoses, underscoring an unmet medical need for improved second-line treatments. Chimeric antigen receptor (CAR) T-cell therapies have emerged as promising options, leveraging engineered autologous T cells to target CD19-expressing lymphoma cells, potentially offering durable remissions or cure.
Study Design
The phase III TRANSFORM study (NCT03575351) is a randomized, open-label global trial comparing lisocabtagene maraleucel (liso-cel), a defined composition CD19-directed CAR T-cell product, to investigator-selected standard-of-care (SOC) therapy as second-line treatment for adults with primary refractory or early relapsed (within 12 months) LBCL eligible for autologous stem cell transplantation (ASCT). Key inclusion criteria required measurable disease, and patients were randomized 1:1 to receive either liso-cel (target dose 100 × 106 CAR-positive T cells) or SOC (platinum-based chemoimmunotherapy followed by high-dose chemotherapy and ASCT if responsive). Bridging therapy was allowed to control disease during manufacturing of liso-cel.
The trial’s primary endpoint was event-free survival (EFS) assessed by an independent review committee (IRC), with secondary endpoints including complete response (CR) rate, progression-free survival (PFS), overall survival (OS), and safety.
Patient Population
A total of 184 patients were randomized and treated (92 per arm). Baseline characteristics were well balanced, including LBCL subtypes, age distribution (median 59 years), disease stage, and prior refractory status. About 66% of eligible SOC patients crossed over to receive liso-cel upon progression or prespecified criteria.
Key Findings
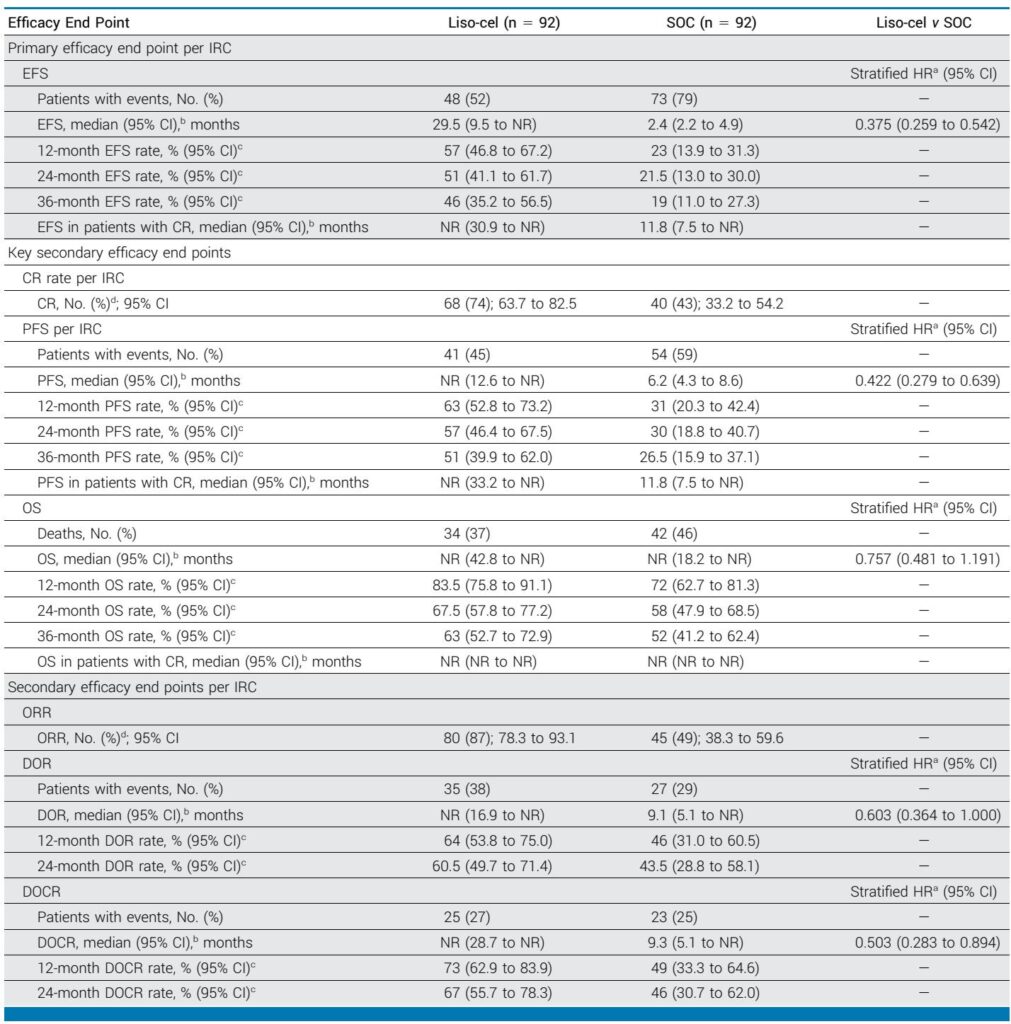
At a median follow-up of 33.9 months, liso-cel demonstrated superior and durable clinical benefit versus SOC:
- Event-Free Survival: Median EFS was 29.5 months (95% CI: 9.5 to not reached) for liso-cel versus 2.4 months (95% CI: 2.2 to 4.9) for SOC, corresponding to a hazard ratio (HR) of 0.375 (95% CI: 0.259–0.542), indicating a 62.5% reduction in risk of event or death.
- Progression-Free Survival: Median PFS was not reached for liso-cel (95% CI: 12.6 to NR) versus 6.2 months (95% CI: 4.3 to 8.6) for SOC (HR 0.422; 95% CI: 0.279–0.639). The 36-month PFS rates favored liso-cel at 51% versus 26.5%.
- Response Rates: The CR rate per IRC was significantly higher with liso-cel at 74% (95% CI: 63.7–82.5) compared to 43% (95% CI: 33.2–54.2) in SOC. The duration of CR was markedly prolonged with liso-cel (median not reached vs 9.3 months in SOC; HR 0.503).
- Overall Survival: Median OS was not reached in either arm; however, 36-month OS rates were 63% for liso-cel versus 52% for SOC. Importantly, adjusted analyses accounting for 66% of SOC patients crossing over to liso-cel showed a survival benefit favoring liso-cel with an HR of 0.566 (95% CI: 0.359–0.895).
Results consistently favored liso-cel across various subgroups, including older patients, those with higher prognostic indices, and different LBCL subtypes.
Safety Profile
Liso-cel exhibited a manageable safety profile in line with prior reports. While prolonged cytopenias (grade ≥3 at 35 days post-infusion) were more frequent with liso-cel, most cases resolved within two months. Rates of severe infections were comparable between arms despite more cytopenias with liso-cel. No new safety signals emerged over extended follow-up. Second primary malignancies were low and balanced between groups. Notably, some grade ≥3 COVID-19-related infections occurred in the liso-cel arm during the post-treatment period, including one fatal case.
Discussion
The 3-year follow-up data from the TRANSFORM trial reinforce that liso-cel provides superior, deeper, and more durable remissions than SOC in patients with high-risk second-line relapsed/refractory LBCL. The magnitude of EFS and PFS improvement, along with higher CR rates and durable responses, underscores the potential of CAR T-cell therapy to change the treatment paradigm beyond salvage chemotherapy and ASCT. The limited OS difference at this time reflects effective crossover and the study not being powered for OS; however, sophisticated statistical adjustments corroborate an OS advantage for liso-cel.
These findings align with earlier reports of CAR T-cell therapies in this setting and extend long-term evidence supporting liso-cel’s curative potential. The safety profile is consistent with known toxicities, and adverse events remain manageable in expert centers.
Limitations include the open-label nature and crossover design impacting OS interpretation, but these are balanced by robust randomized methodology and independent review assessments. The generalizability to broader populations should consider patient selection criteria and availability of specialized CAR T-cell centers.
Conclusion
Lisocabtagene maraleucel significantly improves event-free and progression-free survival with durable complete responses compared to standard second-line therapies in primary refractory or early relapsed LBCL patients eligible for ASCT. The favorable long-term safety and efficacy support liso-cel as a transformative second-line treatment option with potential curative outcomes, warranting integration into clinical practice and future guidelines.
References
Kamdar M, Solomon SR, Arnason J, et al. Lisocabtagene Maraleucel Versus Standard of Care for Second-Line Relapsed/Refractory Large B-Cell Lymphoma: 3-Year Follow-Up From the Randomized, Phase III TRANSFORM Study. J Clin Oncol. 2025;43(23):2671-2678. doi:10.1200/JCO-25-00399