Highlights
- Intra-arterial tenecteplase after successful endovascular therapy increased the likelihood of excellent neurological outcome (modified Rankin Scale 0-1) at 90 days.
- No significant difference in symptomatic intracranial hemorrhage or mortality between groups.
- Secondary efficacy endpoints did not show significant improvement, suggesting cautious interpretation.
- Further large-scale trials are needed to confirm these findings and inform guideline updates.
Clinical Background and Disease Burden
Acute ischemic stroke due to large vessel occlusion (LVO) remains a leading cause of adult disability and death worldwide. Mechanical thrombectomy has revolutionized care for anterior circulation LVO, particularly within the first 6 to 24 hours of symptom onset. Despite successful recanalization—defined as eTICI 2b or greater—a significant proportion of patients do not achieve excellent functional recovery. Microvascular occlusion, incomplete reperfusion at the tissue level, and ongoing thromboinflammation may contribute to suboptimal outcomes. Adjunctive pharmacological strategies to optimize cerebral reperfusion after thrombectomy represent an important unmet clinical need.
Research Methodology
The ANGEL-TNK trial (NCT05624190) was a prospective, open-label, randomized controlled trial with blinded outcome assessment. Conducted across 19 centers in China, the trial enrolled adults with acute anterior circulation LVO stroke who underwent endovascular therapy between 4.5 and 24 hours after last known well. After achieving successful recanalization (eTICI 2b or greater), patients were randomized to receive intra-arterial tenecteplase (0.125 mg/kg) or standard medical management. The primary endpoint was an excellent outcome at 90 days, defined as a modified Rankin Scale (mRS) score of 0-1. Multiple secondary efficacy endpoints included broader functional outcomes (mRS 0-2, 0-3), early neurological improvement, quality of life, imaging-based perfusion/reperfusion markers, and infarct core volume changes. Safety endpoints comprised symptomatic intracranial hemorrhage (sICH) within 48 hours, any intracranial hemorrhage, and all-cause mortality at 90 days.
Key Findings
Among 256 randomized participants (median age 71.6 years; 44.1% female), 255 completed follow-up. At 90 days, 40.5% of patients in the intra-arterial tenecteplase group achieved an mRS score of 0-1 compared to 26.4% in the standard treatment group (relative risk, 1.44; 95% CI, 1.06–1.95; P = 0.02). Importantly, rates of sICH (5.6% vs. 6.2%; RR 0.95, 95% CI 0.36–2.53) and 90-day mortality (21.4% vs. 21.7%; RR 0.76, 95% CI 0.40–1.43) did not differ significantly between groups.
However, none of the seven prespecified secondary efficacy endpoints, including broader mRS dichotomizations, NIH Stroke Scale improvement, quality of life, or imaging metrics, showed a statistically significant advantage for intra-arterial tenecteplase. This disconnect between the primary and secondary outcomes raises important questions about the robustness and generalizability of the primary result.
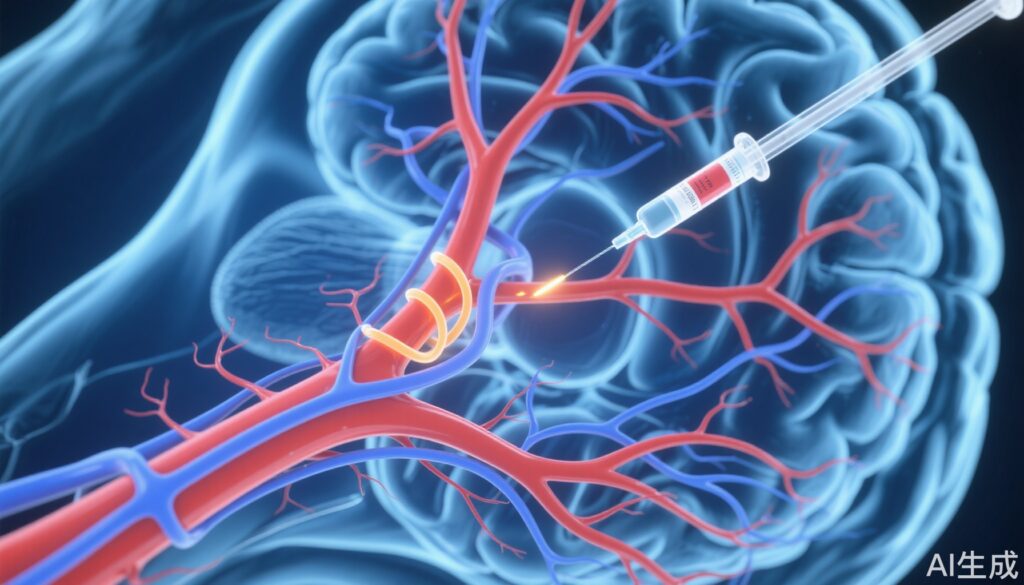
Mechanistic Insights and Biological Plausibility
Tenecteplase, a genetically modified tissue plasminogen activator, offers advantages in fibrin specificity and resistance to plasminogen activator inhibitor-1 compared to alteplase. The intra-arterial route post-thrombectomy may theoretically enhance lysis of residual microthrombi and improve tissue-level reperfusion (no-reflow phenomenon), which is not always addressed by macrovascular recanalization alone. Prior studies have shown mixed results with adjunctive thrombolytics in this setting, emphasizing the importance of route, timing, and patient selection.
Expert Commentary
Current American and European guidelines recognize intravenous thrombolysis prior to thrombectomy in eligible patients, but the evidence for intra-arterial thrombolytics after successful thrombectomy remains limited. As Dr. Raul Nogueira (not involved in ANGEL-TNK) has previously commented, “The focus should be on maximizing tissue-level reperfusion, but we must balance efficacy with bleeding risk.”
Controversies and Limitations
The trial’s open-label design, albeit with blinded endpoint assessment, may introduce performance or detection bias. The sample size, though larger than many previous studies, remains relatively modest for detecting differences in secondary outcomes or rare adverse events. The lack of benefit on secondary endpoints—especially broader functional outcomes and imaging measures—limits confidence in the primary result and suggests the possibility of a chance finding or selective benefit in a specific subgroup. Furthermore, the study population was exclusively Chinese, which may impact generalizability to other ethnic and healthcare settings. The optimal dose, timing, and selection criteria for intra-arterial tenecteplase remain open questions.
Conclusion
ANGEL-TNK provides provocative evidence that intra-arterial tenecteplase after successful endovascular thrombectomy may improve the likelihood of excellent neurological recovery at 90 days, without increasing hemorrhage or mortality. Yet, the lack of benefit across secondary outcomes and potential methodological limitations call for confirmation in larger, diverse populations. For now, intra-arterial tenecteplase should remain investigational, and clinicians should adhere to established guidelines while awaiting further data.
References
Miao Z, Luo G, Song L, Sun D, Chen W, Yao X, Pan Y, Liu Y, Yuan G, Wen C, Wei M, Cai X, Yang Q, Zhou Z, Chang M, Nan G, Wang J, Xiang G, Zhou L, Gao W, Zhang H, Hao J, Xu C, Sun Y, Yi T, Feng G, Han H, Gao F, Ma N, Mo D, Sun X, Deng Y, Tong X, Li X, Jia B, Wang B, He Z, Yang M, Zhao X, Zhang X, Zhang L, Li S, Tong X, Jing J, Xiong Y, Liu T, Li Z, Ren Z, Wang Y, Liebeskind DS, Jovin TG, Nguyen TN, Wang Y, Liu L, Yan B, Huo X; ANGEL-TNK Investigators. Intra-arterial Tenecteplase for Acute Stroke After Successful Endovascular Therapy: The ANGEL-TNK Randomized Clinical Trial. JAMA. 2025 Jul 5:e2510800. doi: 10.1001/jama.2025.10800 IF: 55.0 Q1 .
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke. Stroke. 2018;49(3):e46-e110.
Campbell BCV, Mitchell PJ, Yan B, Parsons MW. Reperfusion after thrombectomy for ischemic stroke. N Engl J Med. 2019;380:1791-1792.